This article discusses primary angle-closure glaucoma, the second most common form of this eye disease. The author discusses important information to know about symptoms, diagnosis, treatment options, known risk factors, and more.
Primary angle-closure glaucoma is associated with closure of the anterior chamber angle of the eye, in contrast to the most common form of glaucoma known as primary open-angle glaucoma. This angle is an important structure in the eye, and is present 360 degrees around the circumference of the eye. The angle can be thought of as the angle between the iris and the cornea, although that is an oversimplification.
Nevertheless, in the angle, one finds the drainage system of the eye, called the trabecular meshwork, which, if your angle is open, is visible to your eye doctor by using a special mirrored lens.
The video below provides a very good representation of the eye’s “angle.”
Video: Angle-Closure Glaucoma
Angle-Closure Glaucoma: What Causes the Eye’s Drainage Angle to Narrow?
In primary angle closure, the trabecular meshwork is not as visible because of a “narrowing” of the angle. There are multiple reasons for this “narrowing.”
-
- Pressure Differences
This includes a pressure difference between the back of the eye (posterior chamber) and the front of the eye (anterior chamber), which can cause the iris to bow forward and cause further angle narrowing. - Anatomical Changes
In far-sighted patients, the eye is shorter than typical, which means the front of the eye is “crowded” and the angle tends to be narrower. Additionally, the thickness of the ciliary body (the part of the eye that produces the eye fluid, called aqueous humor), the position of the iris relative to the ciliary body, the volume of the iris, and the shape, position, and thickness of the lens, all can contribute to angle narrowing.Some of these anatomical features change with age, such as the thickness of the lens, which increases as we get older (forming cataracts). This is why sometimes patients develop progressive angle narrowing over time.In other situations, the closure of the angle can happen acutely, resulting in an acute angle-closure crisis. This is a very worrisome situation in which the eye pressure rapidly increases and vision can be severely affected. We will discuss this important condition later in this article.
- Pressure Differences
Angle Closure: A Few Definitions
First, we will define a few more terms. Angle closure may or may not be associated with increased eye pressure or damage to the optic nerve, and can occur in either an acute or chronic form. Indeed, if one has evidence of angle narrowing but no evidence of increased eye pressure or optic nerve damage, your ophthalmologist may diagnose you as a “primary angle-closure suspect.”
If you have angle narrowing and elevated eye pressure, but no optic nerve damage, you may be diagnosed with “primary angle-closure.”
Finally, if you have angle narrowing, elevated eye pressure, and optic nerve damage, you have “primary angle-closure glaucoma.”
Angle-Closure Glaucoma: Risk Factors
Regardless of the exact diagnosis, the risk factors for primary angle-closure glaucoma include:
- a family history of angle closure
- older age
- female gender
- Asian descent
Other risk factors related to the eye’s anatomy include:
- hyperopia (farsightedness)
- shallow anterior chamber
- thick lens
- short length of the eye
- ciliary body anatomy
Angle-Closure Glaucoma Symptoms
Sometimes angle closure can result in no symptoms, and other times the symptoms are very obvious (as in an acute-angle closure crisis). There can also be intermittent or occasional symptoms, such as blurred vision, halos around lights, eye pain, headache, eye redness, or symptoms occurring after dilation of the eyes. In addition, many medications with glaucoma warnings apply to patients with primary angle-closure. Briefly, these include over the counter decongestants, motion-sickness medications, and anticholinergic agents, just to name a few. Always ask your ophthalmologist about any glaucoma side-effect warnings if you are unsure.
Diagnosis of Angle-Closure Glaucoma
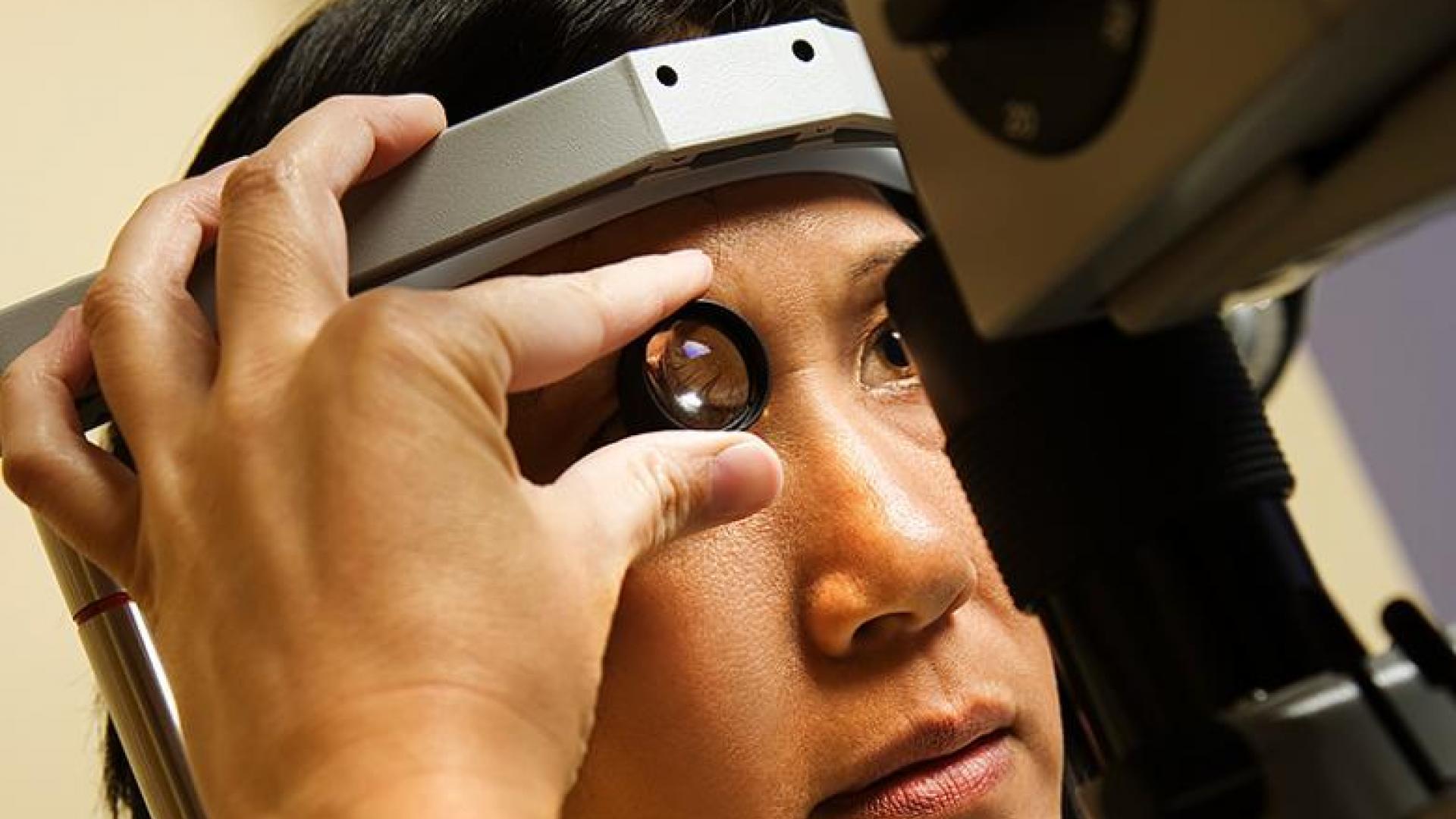
During your eye examination, your eye doctor will assess all parts of the eyes as they would during a comprehensive eye examination, although sometimes a dilated exam will not be performed if your ophthalmologist is very concerned about the narrowness of your angles. In addition, your doctor will perform gonioscopy, which uses a special mirror in order to visualize the angle. Sometimes, imaging of the front part of the eye, called anterior segment optical coherence tomography are, or ultrasound biomicroscopy (a special type of ultrasound eye exam) will be performed to more specifically determine the anatomy of the angle.
Treatment of Angle Closure Glaucoma
After your eye examination, your ophthalmologist will discuss any recommendations for laser peripheral iridotomy, medications, or surgery, which will briefly be discussed below.
Acute Angle-Closure Crisis
In an acute-angle closure crisis, the eye pressure can increase rapidly and to high levels. The patient may experience symptoms such as blurred vision, halos around lights, eye pain, headache, nausea, and possibly vomiting. Untreated, an acute angle-closure crisis can cause permanent vision loss or blindness. In addition, the other eye is at high risk for having a similar crisis. This is why laser peripheral iridotomy is recommended both as a treatment during an acute crisis and in patients who are asymptomatic, but have primary angle closure and are at risk for an acute angle-closure attack.
A laser iridotomy (see video) creates a hole in the iris, which acts as an alternative channel through which eye fluid can flow when the usual pathway becomes blocked.
The risks of the laser iridotomy are relatively low, whereas the harm that an attack can do is relatively high and potentially permanent. In terms of treatment, the initial steps are to break the attack, which will be accomplished using a combination of eye pressure lowering medications and laser iridotomy.
Sometimes removing the lens (or cataract) is recommended in an acute angle-closure crisis. It will be important to discuss with your ophthalmologist the best treatment option for you and your long-term follow-up plan.
Primary Angle-Closure Suspects
Primary angle-closure suspects should have a discussion with their ophthalmologist about the risks and benefits of laser iridotomy, which is a procedure designed to prevent an acute angle-closure crisis. If you need to take medications that might increase your risk of having an attack or you have symptoms that suggest intermittent angle closure, this may push the balance towards undergoing this preventive procedure. Otherwise, sometimes it can be reasonable to follow-up over time to see if the angle becomes progressively more narrow.
Primary Angle-Closure and Primary Angle-Closure Glaucoma
Treatment for patients with primary angle-closure and primary angle-closure glaucoma involves removing a small portion of the outer edge of the iris using laser iridotomy. Patients who have an acute angle-closure crisis in one eye may have treatment performed in the other eye as a precautionary action, as they are at higher risk of having a similar event occurring in the other eye.
Summary
For more information of why an iridotomy helps prevent and/or treat an acute angle-closure crisis, please refer to a detailed article on this topic. Regardless of the specific diagnosis related to primary angle-closure you receive, it is important to discuss with your ophthalmologist the follow-up plan, because chronic forms of the disease can develop and it will be important to catch this earlier rather than later.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Medications
- Treatments









