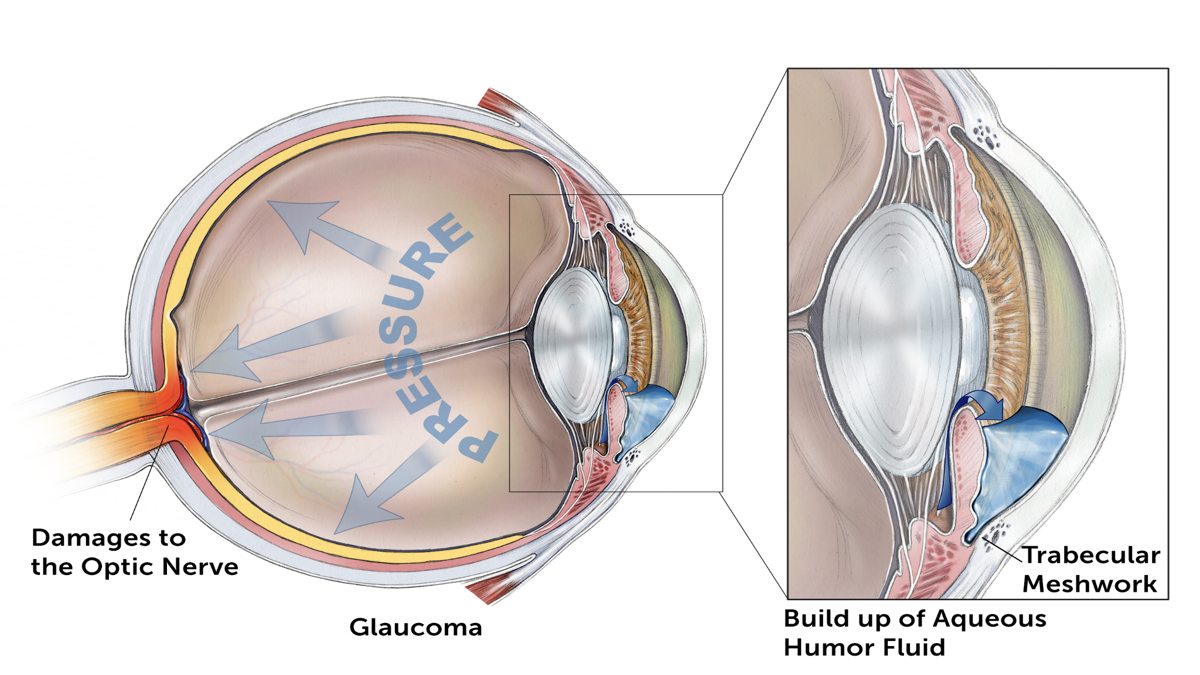
Glaucoma is a group of eye diseases that can damage the optic nerve and result in vision loss and blindness. In all forms of glaucoma, the status of the eye’s drainage system, the trabecular meshwork, is important.
Learn how the eye’s drainage system relates to the development and treatment of glaucoma.
New drugs on the horizon may directly target the trabecular meshwork, which is very exciting. A new class of glaucoma medications would be a welcome addition, since some patients do not respond to current medications.
A Most Important Angle
The “angle” referred to here is the angle between the iris, which makes up the colored part of your eye, and the cornea, which is the clear-window front part of your eye. When the angle is open, your ophthalmologist can see most, if not all, of your eye’s drainage system by using a special mirrored lens. When the angle is narrow, only portions of the drainage angle are visible, and in acute angle-closure glaucoma, none of it is visible.
The angle is the location where the fluid that is produced inside the eye, the aqueous humor, drains out of the eye into the body’s circulatory system. The function of the aqueous humor is to provide nutrition to the eye and to maintain the eye in a pressurized state. Aqueous humor should not be confused with tears, since aqueous humor is inside the eye.
One of the main structures of the drainage angle, the trabecular meshwork, plays a very important role in the drainage of aqueous humor. The majority of fluid draining out of the eye is via the trabecular meshwork, then through a structure called Schlemm’s canal, into collector channels, then to veins, and eventually back into body’s circulatory system.
What is the Trabecular Meshwork?
The trabecular meshwork is the spongy tissue located near the cornea through which aqueous humor flows out of the eye. The trabecular meshwork lies in the drainage angle (see video above), and 80 – 90 percent of aqueous humor makes its way into circulation via the trabecular meshwork and its associated structures. Ophthalmologists and scientists believe that one particular part of the trabecular meshwork is the site of greatest resistance to aqueous humor outflow. If there is higher outflow resistance, then the eye pressure gradually increases.
Watch: The Eye’s Drainage System in Action
The Impact of Age
One may wonder why the risk for glaucoma increases with age. One explanation is that with increasing age, we lose trabecular cells, which have a role in keeping the trabecular meshwork functioning well. One may also ask the opposite question: why are some babies born with congenital glaucoma? In this case, there may be abnormal development of the trabecular meshwork, such that it does not function properly. Clearly, the trabecular meshwork plays a very important role, and some even call glaucoma a “trabecular meshwork disease.”
Treatments for the Eye’s Drainage System
Medications
How do glaucoma treatments affect the trabecular meshwork? The currently available medications either decrease aqueous humor production (“turning down the faucet”) or increase aqueous humor outflow via a pathway that does not directly involve the trabecular meshwork. However, new drugs that were approved in late 2017 (Vyzulta™ and Rhopressa®) directly target the trabecular meshwork, which is very exciting, since these are the first new glaucoma drugs in over two decades. In addition, these drugs directly target the diseased trabecular meshwork! The year 2018 will be very exciting as we see how these new medications actually work in everyday patients.
Lasers
Laser trabeculoplasty (selective laser trabeculoplasty, SLT, as one example) targets the trabecular meshwork. Once these cells are activated, they release molecules that help improve outflow via the trabecular meshwork and its associated structures, thereby lowering eye pressure.
New Surgical Techniques
Finally, this is also an exciting time in the development of new surgeries for glaucoma, as some of these new surgeries target the trabecular meshwork and its associated structures.
Some of these surgeries are termed “minimally invasive or micro invasive glaucoma surgeries” (MIGS), and some are being paired with cataract surgery to lower eye pressure and/or decrease the number of medications patients need to use in early to moderate-stage glaucoma.
One such surgery using the Trabectome device targets the trabecular meshwork and removes it, opening access to Schlemm’s canal as a way to lower eye pressure.
Another surgery uses the iStent, a very tiny titanium stent that makes an opening into the trabecular meshwork, thereby bypassing it and allowing fluid to flow into Schlemm’s canal and lower eye pressure.
The CyPass® micro-stent, which is combined with cataract surgery to lower eye pressure by bypassing the trabecular meshwork altogether was voluntarily removed from the market In 2018 by the manufacturer. Learn why the manufacturer took this step, and what you should do if you have already had the CyPass micro-stent procedure.
Finally, Xen is a very small gel stent that can be performed as a standalone procedure by itself, and is less invasive than standard trabeculectomy surgery. However, its effectiveness has not yet been measured directly against trabeculectomy.
While these surgeries are not suitable for everyone, and often do not achieve the very low eye pressures that some patients require, it is a promising time in the development of new treatments targeting or bypassing the trabecular meshwork, and therefore glaucoma.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Eye Health
- Eye Pressure









