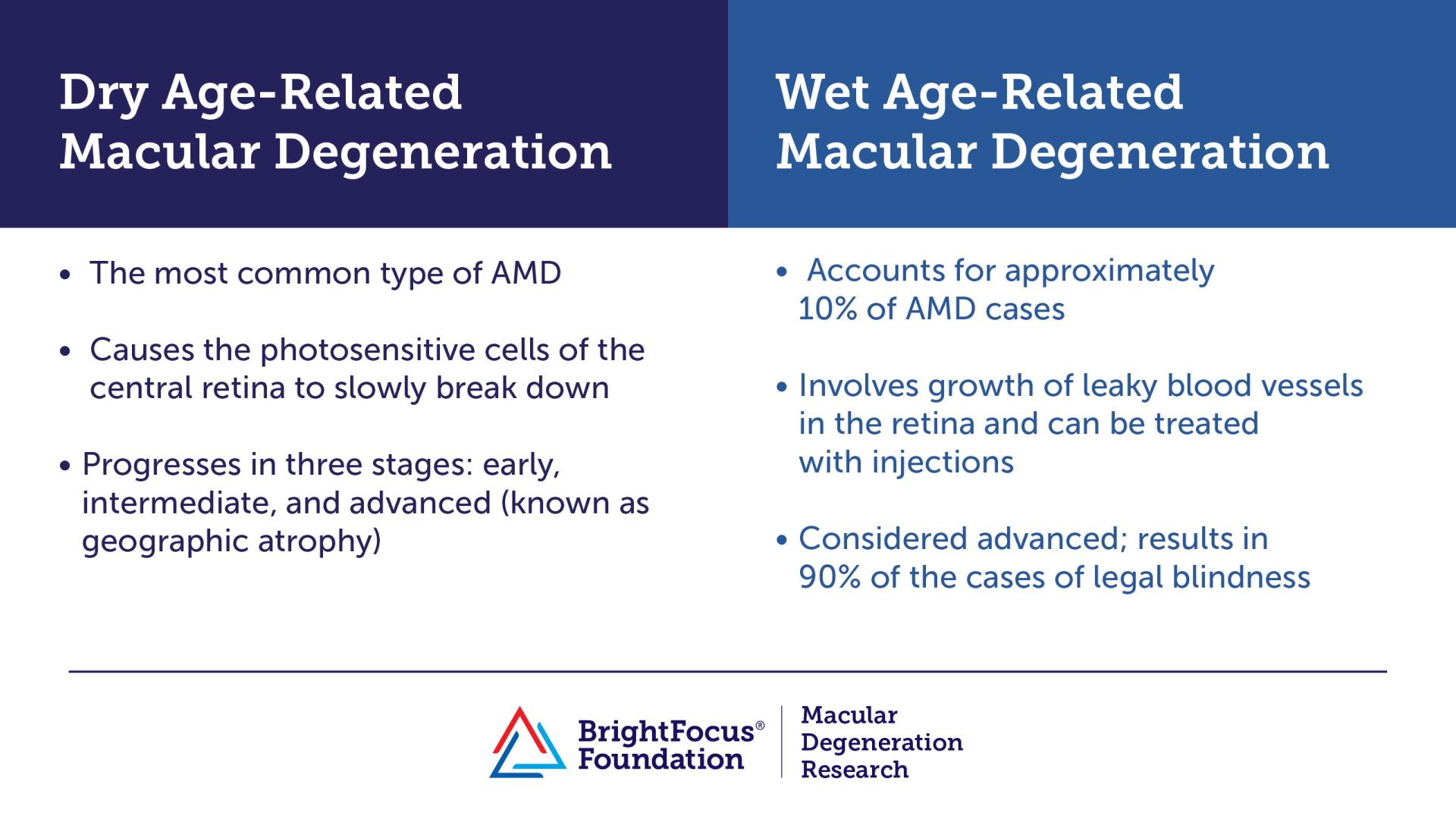
- The two types of age-related macular degeneration (AMD) are dry and wet. Both forms can cause vision loss.
-
Dry AMD may advance and cause vision loss with or without turning into the wet type of the disease.
-
Wet AMD is considered advanced and involves growth of leaky blood vessels in the retina.
Patients often ask, is my age-related macular degeneration (AMD) wet? This is an important question since it affects the rate of vision loss and treatment. The most common type of macular degeneration, about 85 to 90 percent of cases, is the dry (atrophic) type. Dry AMD is divided into two main categories: early and late. In the late category, patients can have wet AMD, geographic atrophy, or both. All wet AMD is considered advanced.
Early Dry AMD
Patients can start to develop early dry AMD at age 55 or older (rarely younger). This stage is often asymptomatic or mildly symptomatic. Symptoms can include slight distortion of central vision or difficulty with dark adaptation—as with looking for seats when walking into a dark theatre. It is diagnosed by an ophthalmologist who can see tiny white spots in the retina called drusen. This is a German word meaning “geode,” and they’re like little pebbles under the retina. The pebbles are made of fats, proteins, and minerals that deposit under the retina over time. In some ways they are similar to thickening or hardening of arteries.
Drusen can be small or large, few or numerous. If they are found in one eye, they will usually be in the other eye too. Large, numerous drusen indicate a higher risk for future vision loss. However, it’s reassuring that many patients with drusen never progress to late AMD and are able to keep good vision throughout their lives. Even those who develop late AMD can keep good vision, especially with the treatments described below.
Drusen can be viewed with an ophthalmoscope or with special lenses by an ophthalmologist or optometrist during a dilated eye exam. They can also be photographed using a technique called fundus photography or imaged using a device called optical coherence tomography (OCT). These images can be used to compare the number and size of drusen over time. In some cases, large drusen in the center of the retina can cause some vision distortion. We don’t have a proven method to eliminate drusen, but one study from Massachusetts Eye and Ear provided some evidence that certain doses of specific statin drugs may help shrink large drusen in the center of the retina.
Patients with early AMD can reduce their risk of progression to wet AMD by about 25% if they take antioxidant vitamins following the age-related eye disease study (AREDS 2) formula. The best validated of these vitamins is marketed by Bausch & Lomb under the brand Preservision. These vitamins, while available over the counter, should only be taken if recommended by an eye care professional. Not all patients with early AMD need them, especially if they have few or small drusen.
Patients with early AMD can also reduce their risk of central vision loss by avoiding smoking and eating a healthy diet. Several epidemiological studies show that a low-risk diet includes fruits and vegetables (especially dark green leafy vegetables like spinach, kale, and collard greens), fatty fish like salmon twice a week, minimal snack foods with unhealthy oils, minimal sugar, and minimal red meat. They should also monitor their disease at least annually with a visit to an ophthalmologist and by checking their central vision on the Amsler grid.
The Amsler grid looks like a piece of graph paper. It should be used with reading glasses on. One eye should be closed to check each eye independently. Looking at the dot in the center, it should be noted if any of the lines on the graph are missing or wavy. This is especially concerning for late AMD if it looks different from the appearance at the time of the last ophthalmologist visit. Automated Amsler grids are now available.
Wet AMD
Wet AMD means that new blood vessels have grown into the retina. The vessels leak and bleed, causing fluid to accumulate within the retina, making it “wet.” This leakage can cause sudden distortion or loss of central vision, which patients can notice using an Amsler grid. Or, they may notice difficulty reading or seeing faces, especially with the “good” eye closed. Objects that should appear straight may look curved. Fluid in the retina can be detected by the ophthalmologist with non-invasive, rapid OCT imaging.
The blood vessels are thought to grow because of decreased oxygen levels in the retina or inflammation. Either of these can cause an increase in blood vessel growth proteins including vascular endothelial growth factor (VEGF). If left untreated, wet AMD usually causes scarring of the central retina (macula) with permanent central vision loss. Because of this, it’s very important for patients to have wet AMD treated within about a week of onset and continue their treatments as directed by their ophthalmologist.
Drugs In Development
Fortunately, drugs have been developed that block VEGF. Four drugs have been FDA-approved for injection into the eye. These drugs typically need to be injected every 1-3 months, depending on whether blood vessels are still leaking. These are called Eylea, Vabysmo, Lucentis, and Beovu. Vabysmo also blocks another blood vessel-promoting protein called Ang2.
Unfortunately, Beovu causes rare but potentially blinding blood clots in the eye. The other drugs have not been associated with this side effect. Eylea and, especially Vabysmo, can last longer than Lucentis. Please discuss with your doctor what the best treatment options are for you.
Longer-lasting gene therapies are also in clinical trials. Following FDA approval of the drug Luxturna, developed at the University of Pennsylvania for hereditary blindness, there is now much interest in developing gene therapy for additional diseases. One of these, called RGX-314, is now in phase 3 clinical trials and has the potential to keep wet AMD at bay after only a single injection in the operating room.
Geographic Atrophy
The late and most advanced stage of dry AMD is geographic atrophy (GA). This occurs when the light sensing photoreceptor cells die. Typically, they will die in a small patch or patches, which then expand slowly over time. This causes blind spots near the center of vision that expand over months to years. Until recently, there was no treatment for GA other than vision aids prescribed by an optometrist who specializes in low vision. These types of aids can include glasses with high magnification, special lights, and electronic devices that magnify objects or letters.
Now, successful clinical trials are supporting an application to the FDA for a new treatment. This treatment, currently called Apl-2 (pegcetacoplan) is injected into the eye every month or two. It can slow the rate of GA expansion by about 20% over the first year, but the degree of protection seems to increase over time. This treatment is under FDA Priority Review and, if approved, may become available in 2023.
Apl-2 targets a protein called complement, which is a part of the immune system. Genetic evidence implicates several complement proteins in AMD. Together these form a chain called the complement cascade that can increase inflammation, cell death, and even lipid contents in the retina. Another drug, Zimura, also targets one of the complement proteins and may receive FDA approval in late 2023.
Overall, the pace of new knowledge about AMD and development of new drugs is increasing! These, combined with lifestyle modifications, may help many people keep good central vision throughout their lifetimes.
Want to learn more about the latest research developments in age-related macular degeneration? Join an upcoming BrightFocus Chat, free monthly telephone discussions with scientists and eye experts about managing vision loss and exciting scientific breakthroughs.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Dry AMD
- Wet AMD









