This article explores the most common early sign of macular degeneration. Learn what drusen are, why the size and number of drusen is important, and more.
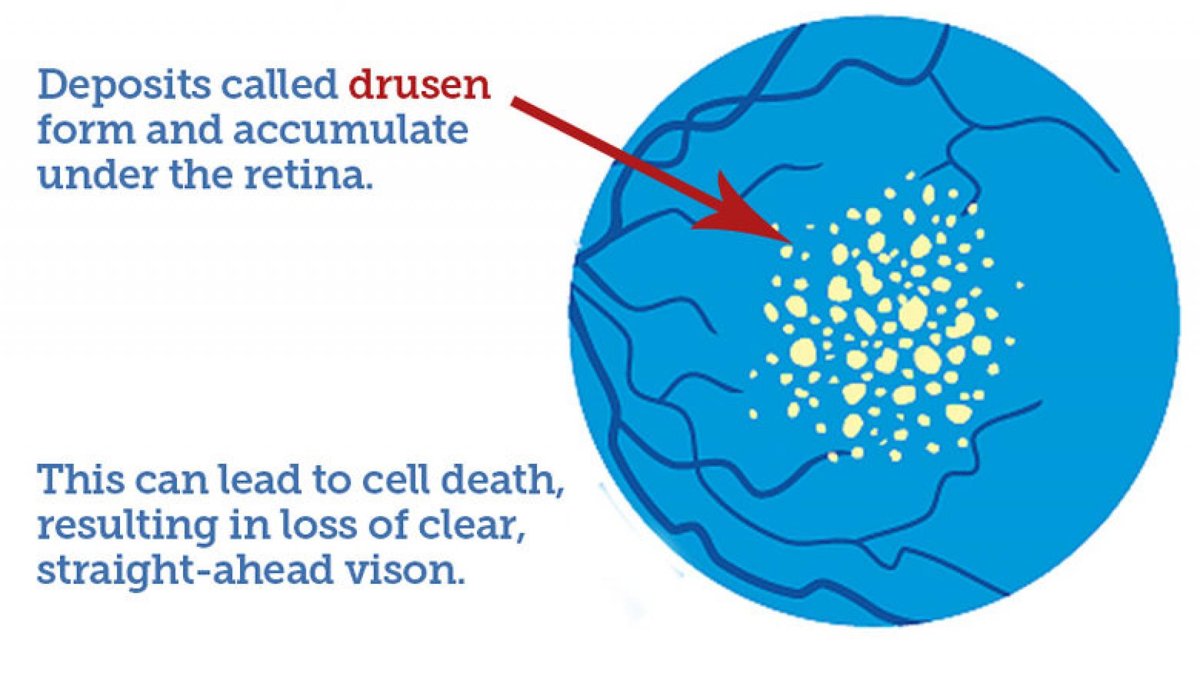
Drusen are the defining feature of macular degeneration. These small yellow or white spots on the retina can be detected by an ophthalmologist during a dilated eye exam or with retinal photography. People with more than a few small drusen are said to have early age-related macular degeneration (AMD). People with drusen often may not experience symptoms. Rather, the existence of these deposits represent a risk for some degree of vision loss in the future. The only way that you can know for sure if you have drusen is from a thorough eye examination.
What are Drusen?
Drusen is a German word that means “rock” or “geode.” They are like tiny pebbles of debris under the retina. The cause of the drusen deposits is related to a type of “garbage” disposal problem. Retinal cells dump unwanted material, and immune cells normally clean up most of it. However, if too much is dumped, or it is not properly packaged for disposal, or the immune cells don’t function efficiently, it can pile up. The drusen contain proteins and lipids (naturally occurring molecules that include fats). Some of the proteins are pro-inflammatory, indicating that the immune system is coating the drusen. One protein in drusen is beta amyloid, which is also found in deposits within the brains of people who have Alzheimer’s disease, and may contribute to both diseases. Fortunately, having AMD is not a major risk factor for developing Alzheimer’s disease.
Video on Dry Macular Degeneration
Size and Number of Macular Drusen
The risk of future vision loss is related to the number and size of the drusen. People with more drusen, and larger drusen, are at higher risk than those with fewer, smaller drusen. Drusen are categorized as small, intermediate and large. This is important, because patients with about 20 or more intermediate drusen or at least one large “druse” were found to benefit from taking the AREDS2 antioxidant vitamins (lutein, vitamin C, vitamin E, zinc and copper). Taking these antioxidant vitamins significantly reduced the risk of vision loss.
The presence of drusen means that some central vision loss could occur in the future, either from slowly progressing atrophy (shrinking or withering away of the retinal tissue), called geographic atrophy, or from rapid new blood vessel growth and leakage, called neovascularization, which occurs in wet age-related macular degeneration (AMD).
Monitoring for Wet AMD
To monitor for the onset of wet AMD, patients with drusen are given an Amsler grid. To use this, close one eye at a time, and, wearing reading glasses, keep the grid at book-reading distance and look at the dot in the center. If the lines look wavy, or some part of the grid is missing, call your ophthalmologist for an appointment, as wet AMD is best treated soon after its onset. Sometimes large drusen can cause waviness of Amsler grid lines. If your doctor tells you that you do not have wet AMD, but you still see some waviness, this may be due to the drusen. In that case, look for a change in the appearance of the grid over time.
The ForeseeHome Monitor® from Notal Vision® is the first FDA-cleared device for patients with dry AMD to monitor the disease at home. It is now a Medicare-covered service for patients enrolled in Medicare across the U.S., and who meet the eligibility criteria for dry AMD at high risk for converting to wet AMD. The device is designed to be used daily and takes approximately 3 minutes per eye. When used daily, the ForeseeHome Monitor detects changes before a patient would notice, and allows the doctor to monitor the vision for any changes that take place between regularly scheduled exams. In a clinical trial that involved over 1500 participants, the device demonstrated that 87-94% of users maintained 20/40 vision or better at the time of wet AMD detection, compared to only 62% of those who used conventional methods such as the Amsler grid. Vision at this level is significant because vision that is better than 20/40 allows patients to maintain their usual level of independence. They are able to read, maintain their driving license and continue to function at a very high level. A separate monitoring center processes each test and your prescribing doctor receives a monthly report. If there is a deviation from the usual testing, an alert would be triggered that would inform the prescribing doctor of a change that may be suggestive of wet macular degeneration. The prescribing doctor would then do a complete eye examination to assess if there has been a change to wet AMD. Learn more about monitoring the progression of dry AMD.
Summary
It is not known whether drusen themselves cause AMD, or if they are just a sign that the retina is not functioning properly. Several studies have investigated whether drusen removal could decrease the risk of vision loss. Over a decade ago, it was discovered that certain laser treatments could cause drusen to shrink or disappear. Later, several clinical trials showed that the drusen-shrinking laser treatments did not improve the chances of keeping stable vision.
The good news about drusen is that many people who have them are able to keep good reading and driving vision throughout their lives, since many people with drusen will not get wet AMD, and those who do can often have their vision protected by injection of medicines that prevent the growth of abnormal, leaky blood vessels. Geographic atrophy, the other potential cause of vision loss in people with drusen, is a major focus of current research, and promising treatments are in the pipeline.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Wet AMD









