Sorsby’s fundus dystrophy is a rare form of inherited retinal degeneration. It can appear similar to age-related macular degeneration (AMD), especially in its early stages. People with AMD have drusen, which are yellowish-white spots under the retina detected by an ophthalmologist during a dilated eye exam. People with Sorsby’s can also have drusen-like deposits, leading them to be diagnosed initially with AMD.
How is Sorsby’s Different from Age-Related Macular Degeneration?
Sorsby’s often progresses more rapidly and requires more frequent monitoring and treatment than AMD. One clue suggesting the possibility of Sorsby’s is a strong family history of macular degeneration since Sorsby’s is inherited in a dominant manner. A dominant genetic trait is expressed in a person even if they have only one copy of that gene. AMD also has a hereditary component, so family history alone is not enough to make the Sorsby’s diagnosis.
Earlier onset can also suggest Sorsby’s. Patients with Sorsby’s can begin to have drusen-like retinal deposits in their 40s, while AMD usually begins between the ages of 50 and 70. Difficulty with dark adaptation (seeing in a dark room immediately after coming in from a bright area) or night blindness can be prominent symptoms in Sorsby’s (but slow dark adaptation can also occur in AMD). Other symptoms in Sorsby’s and AMD can include distorted/reduced central vision.
Diagnosis
A retinal imaging test called an ICG angiogram, which can be done in a retina specialist’s office, can help to diagnose Sorsby’s, since it appears unusually dark, even in young, asymptomatic people who carry the Sorsby’s gene. The definitive diagnosis can be made using genetic testing.
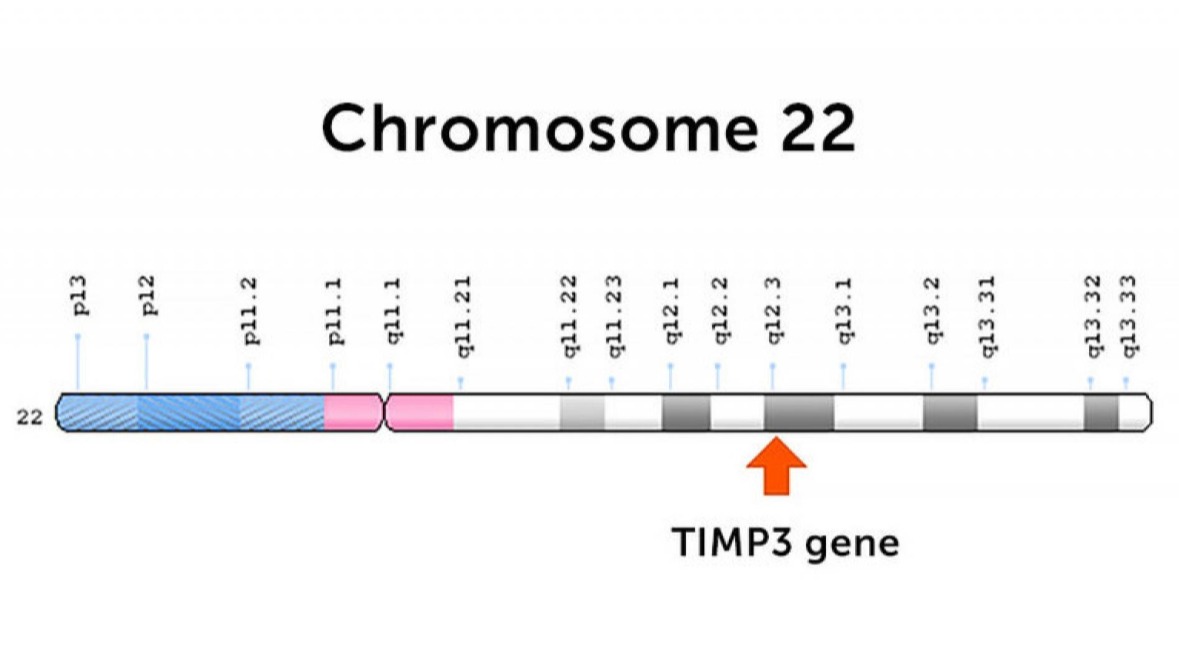
Patients with Sorsby’s have dominant mutations in the TIMP3 gene, which is located on chromosome 22. This gene is expressed in the retina, and normally helps maintain a thin membrane that separates the retina from its underlying blood vessels. When the gene is mutated, the retinal pigment epithelial cells sitting in the membrane can die, or the membrane can be penetrated by abnormal blood vessels that leak and bleed.
Treatment
Abnormal new blood vessels in patients with Sorsby’s can be treated in the same way as those in wet AMD: by injections into the eye of anti-VEGF antibodies such as Avastin. These injections can stop harmful leakage from the abnormal blood vessels.
Sorsby’s patients who lose vision can be aided by a low vision specialist. These optometrists are specially trained to provide optimal glasses, lights, magnifiers, and electronic devices, along with patient training to make the best use of their existing vision.
Hope for the Future
Currently, there are no other effective treatments for Sorsby’s, but recent advances in gene therapy for the retina, including FDA approval for Leber congenital amaurosis (LCA), a different form of inherited blindness, provide hope for a genetic therapy in the future. Since Sorsby’s is a dominant disease, gene therapy is more difficult, but recent advances in genetic therapies, like CRISPR/Cas, suggest that even dominant retinal diseases may be treatable after further cutting-edge research.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Eye Health
- Genetics









