Learn about a recent gene therapy breakthrough and how that may open the door for new treatments for retinal diseases, including macular degeneration.
A Gene Therapy Breakthrough
There is a new breakthrough in gene therapy, with the FDA recently approving the first gene to be injected into people to treat a disease.
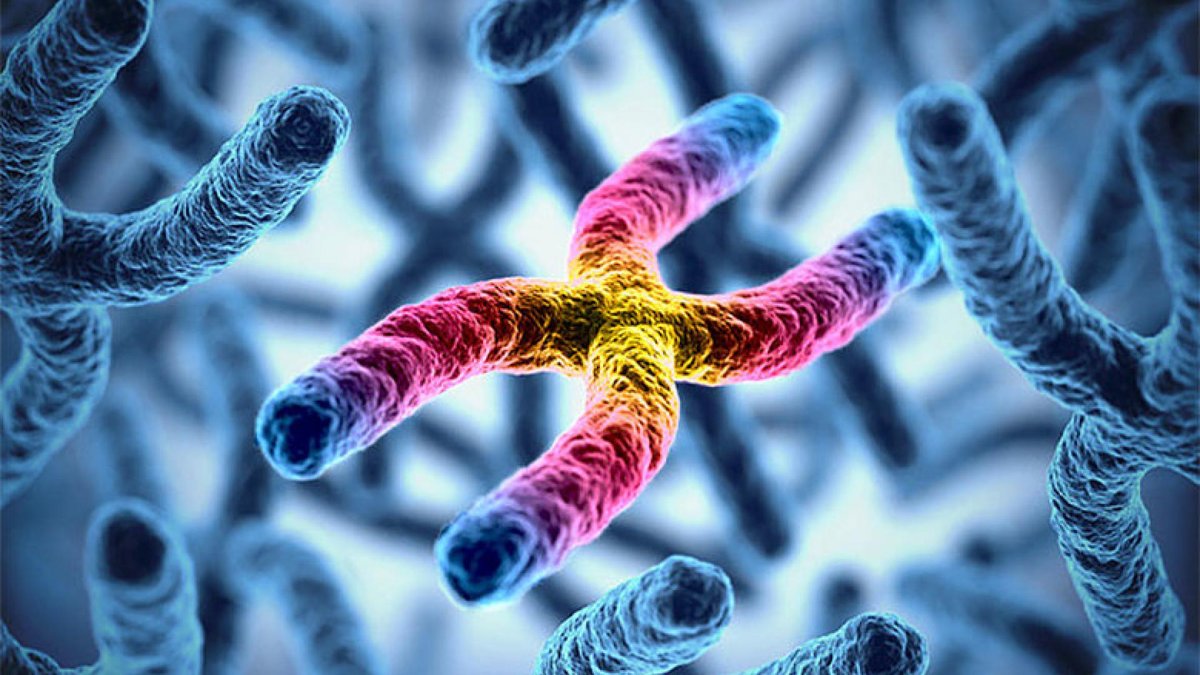
Scientists researching a form of inherited blindness in children called Leber’s congenital amaurosis recently had success in a clinical trial that improved the vision of children in the study. The trial was preceded by 30 years of research by Jean Bennett and her husband, Al Maguire, at the Scheie Eye Institute of the University of Pennsylvania, as well as other scientists at Penn and around the world.
The gene, which is called RPE65, is injected into the eye, under the retina, in an operating room procedure performed by Dr. Maguire. The gene enters retinal cells because it is packaged into a safe virus called adeno-associated virus (AAV). Neither the naturally occurring AAV nor the genetically modified version designed to carry the RPE65 gene into people causes disease. On the contrary, the genetically modified AAV was able to significantly restore vision in blind children, enabling them to complete tasks such as walking through a maze without bumping into soft objects, or catching a ball.
Paving the Way for Other Eye Diseases
The retinal RPE65 gene therapy is a breakthrough that will pave the way for gene therapies treating a number of other retinal diseases, including age-related macular degeneration (AMD), retinitis pigmentosa, choroideremia, and others. Now that a safe and effective technique has been established for delivering a gene into the retina, additional genes can now be delivered to the retina in the same way and tested for efficacy and safety in clinical trials.
Challenges do remain, however. Some genes, such as the one causing Stargardt’s hereditary maculopathy (an inherited disorder of the macula that typically causes vision loss during childhood or adolescence), are too large to be carried into the retina by the AAV virus, so other approaches must be developed. For example, a clinical trial is evaluating another type of virus, called lentivirus, which can carry larger genes. For some complex diseases, such as AMD, it is not as clear which genes will protect vision.
Wet AMD
Early stage clinical trials have used adeno-associated virus to deliver genes encoding VEGF blockers similar to Lucentis and Eylea. One drug called RGX-314 is injected under the retina in the operating room. In a phase I/2 trial, the therapy was safe and appeared to nearly eliminate the need for additional treatments over a one-year period. Another drug called ADVM-22 is injected into the vitreous jelly in the center of the eye instead of under the retina. This is an office procedure. This drug also dramatically reduced the need for additional treatments, and some patients have gone for at least a year without the need for anti-VEGF drug injections. It can cause inflammation, but this has responded to treatment with steroid eye drops.
Dry AMD
Gene therapy for dry AMD is not yet as far along as that for wet AMD. However, it is likely to be helpful after further research and development. Genetic, biochemical, and cell biology studies have identified a number of potential approaches to treat dry AMD, such as anti-inflammatory, anti-oxidant, anti-cholesterol, and anti-cell-death approaches. Some of these have proven effective in gene therapy studies in mice.
A Word of Caution
A potential downside of gene therapy is that, in most cases, it will not be possible to turn off the therapy once it is delivered into the eye. The cells that receive the therapeutic genes will continue to express them for years. Therefore, clinical trials are very important to determine the long-term safety of this approach. Fortunately, the pioneering gene therapy trials for Leber’s congenital amaurosis do not have long-term safety issues, and are restoring some vision in children who were born blind!
The Search for a Cure
Learn how BrightFocus Foundation is funding cutting-edge research to find new cures and treatments for macular degeneration.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Medications