
Understanding Macular Degeneration

What is Macular Degeneration?
Macular degeneration is a disease of the retina that affects the macula in the back of eye. The disease is most common in people over age 60, which is why it is often called age-related macular degeneration (AMD). As many as 20 million people in the U.S. have some form of AMD.
AMD causes deterioration in the central area of the retina, called the macula, which provides the sharply focused central vision needed to read, recognize people and objects, and perform skilled tasks. Damage to the macula results in blind spots and blurred or distorted vision.
Dry AMD
All AMD starts as the dry form. Yellow waste deposits called drusen build up under the retina, and cells of the macula may slowly break down as a result.
Dry AMD occurs in three stages: early, intermediate, and advanced. There may be no symptoms in the early stages, but as the disease progresses, a blurry spot may appear in the center of vision that can grow larger and darker, resulting in a complete loss of central vision.
Dry AMD can reach an advanced stage that leads to vision loss, also known as geographic atrophy (so named because macula cells begin dying in clusters that resemble countries on a map).

Wet AMD
Wet AMD is usually preceded by the dry form. As the condition worsens, abnormal blood vessels grow behind the macula. They can leak blood and fluid, damaging the macula and leading to distorted vision.
In wet AMD, straight lines may appear wavy and central vision loss can occur rapidly— sometimes within days.
The wet form, always considered the advanced stage of the disease, accounts for approximately 10% of all AMD cases but causes 90% of AMD-related blindness.
As with dry AMD, people with advanced wet AMD may develop a large blurry spot in the center of the visual field that expands and darkens, eventually destroying central vision.
Early Diagnosis Can Protect Sight
It’s important to get comprehensive, dilated eye exams as recommended by your eye doctor. In these exams, the pupil is dilated with eye drops to allow your eye doctor to see into the retina.
Because some eye diseases can begin in midlife but may not noticeably affect vision until later, the American Academy of Ophthalmology recommends people age 40 and older get a baseline comprehensive eye exam, with follow-up eye exams every one or two years or as indicated by the eye doctor.

Treatments
People with intermediate-stage dry AMD may benefit from taking the right mix of vitamin supplements to decrease their risk of losing central vision.
The National Eye Institute sponsored studies, including the Age-Related Eye Disease Study (AREDS) 2, which showed that the specific vitamin formula below may slow the risk of dry AMD progression from intermediate to advanced stages, where it can cause vision loss.
Wet AMD is most commonly treated by injecting drugs known as angiogenesis inhibitors into the eye, which block the activity of a protein known as vascular endothelial growth factor (VEGF). In the U.S., several drugs in this “anti-VEGF” class have been used for wet AMD treatment.
For more details, download our Macular Degeneration Treatments fact sheet at brightfocus.org/macular/treatments.
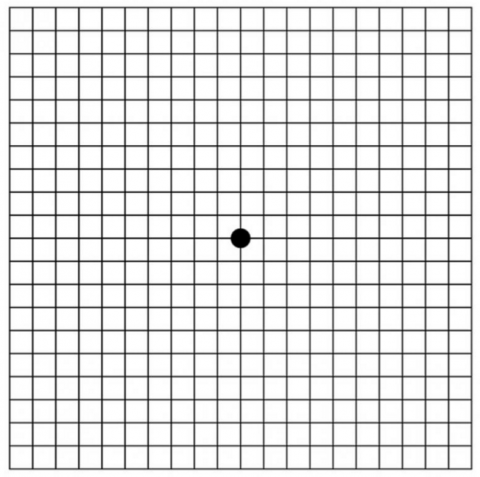
Amsler Grid
In addition to regular eye exams, home monitoring has been proven to improve detection of age-related macular degeneration.
Dry AMD can turn into wet AMD rapidly, which can accelerate vision loss. You can use a special tool called the Amsler grid to evaluate your vision daily at home. The tool uses a simple grid pattern to show spots in your field of vision.
Request a free Amsler grid by calling 1-855-345-6637 or visit brightfocus.org/amsler to download a free printable PDF. If you notice changes in your vision, alert your eye doctor immediately.
Reducing Your Risk
Healthy habits improve overall health, may reduce the risk of developing AMD, and help protect remaining vision for those with AMD. Everyone should practice these habits to support eye health:
- Maintain a healthy weight.
- Eat a varied and nutritious diet, including green leafy vegetables, yellow and orange fruit, fish, and whole grains.
- Don’t smoke.
- Maintain normal blood pressure and control other medical conditions.
- Exercise regularly.
- When outdoors, wear a hat and sunglasses with UVA and UVB protection.
BrightFocus is at the forefront of innovative global brain and eye research, promoting better health through our three programs: Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
