Learn about a glaucoma laser treatment that targets the part of the eye that produces eye fluid.
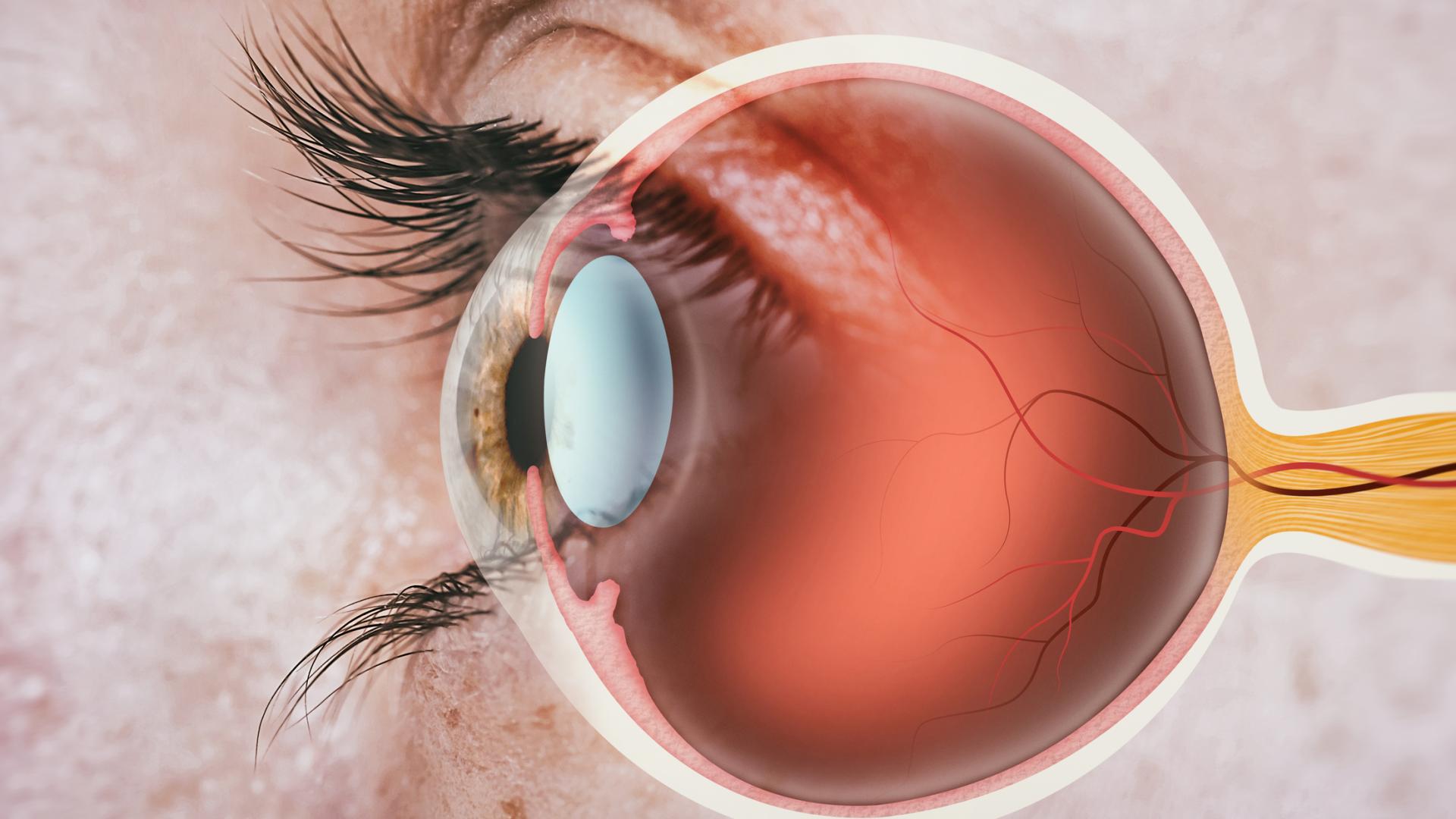
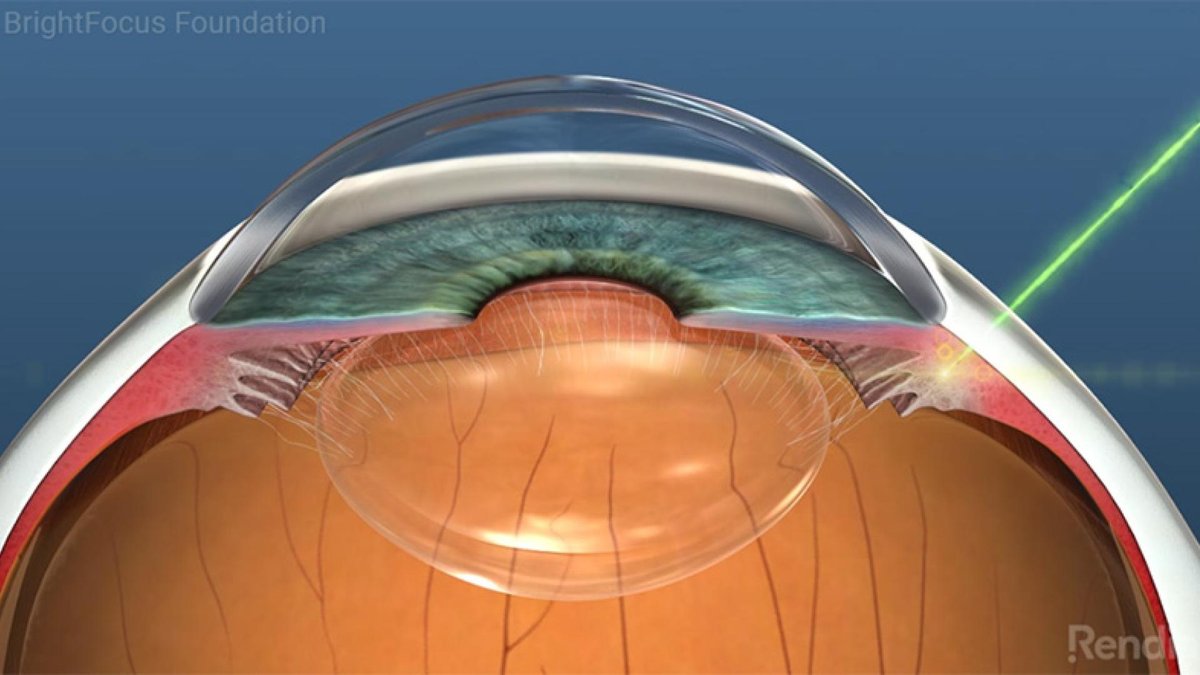
Cyclophotocoagulation is a laser treatment that targets the ciliary processes of the eye. The ciliary processes are the part of the eye that produce the fluid, or aqueous humor, that bathes the tissues in the front of the eye.
Although the part of the eye that does not function well in glaucoma is the “outflow” or drainage system, including the trabecular meshwork, many treatments target the “inflow” system, such as the ciliary processes which form a ring 360 degrees around the circumference of the eye. For example, timolol, a commonly used glaucoma medication, actually lowers eye pressure by targeting the ciliary processes and reducing the amount of aqueous humor that is produced. Utilizing the same concept, cyclophotocoagulation is a laser treatment that targets the ciliary processes to reduce aqueous humor production.
How Does Cyclophotocoagulation Work?
The cyclophotocoagulation laser treatment causes the ciliary processes to shrink, resulting in less aqueous humor production and lower eye pressure. However, the ciliary processes can regenerate, so sometimes the procedure needs to be repeated. In addition, because this procedure causes destruction of the ciliary processes, it was generally reserved after other surgeries, such as trabeculectomy or tube shunt surgery, had been attempted. These surgeries bypass the diseased outflow system by creating a new path for fluid to escape the eye. However, in more recent years, cyclophotocoagulation has been used earlier in the treatment algorithm, particularly with the development of different laser techniques that cause more targeted tissue treatment and/or less inflammation.
Types of Cyclophotocoagulation
Transscleral Diode Cyclophotocoagulation
The standard cyclophotocoagulation treatment is called “transscleral diode cyclophotocoagulation.” In this surgery, an 810-nm (nanometer) diode laser probe is placed on the surface of the eye on the sclera, and “spots” of laser treatment are applied. There are no incisions made into the eye, so there is no risk of infection. However, the eye does typically need a type of anesthesia that is easier to administer in the operating room, although it can be done in the clinic setting as well.
Micropulse Transscleral Cyclophotocoagulation
More recently, a newer laser modality called “micropulse transscleral cyclophotocoagulation” has become available and more widely used. In this surgery, an 810-nm diode laser probe is placed on the surface of the eye on the sclera, and there are no incisions made. However, the laser energy is “chopped up” into little pulses or “micropulses,” and this results in less inflammation and potentially less “collateral damage” to other tissues of the eye.
Endocyclophotocoagulation
Finally, endocyclophotocoagulation also utilizes an 810 nm laser probe, but instead of applying the treatment on the outside surface of the eye, this surgery requires an incision into the eye, and the laser probe has a camera that allows the surgeon to directly visualize the ciliary processes. This provides some obvious advantages because the surgeon can directly target the ciliary processes. Some surgeons consider this surgery a MIGS (minimally invasive glaucoma surgery) procedure and may combine it with cataract surgery.
Watch a Video on Endoscopic Cyclophotocoagulation
Who Should Have Cyclophotocoagulation?
As mentioned earlier, traditional cyclophotocoagulation was reserved after other surgeries had been attempted or only in eyes that did not have good vision. However, with the advent of micropulse cyclophotocoagulation and endocyclophotocoagulation, these surgeries are being used earlier in the treatment process.
In general, all forms of glaucoma can potentially be treated using cyclophotocoagulation, although different types of glaucoma have special considerations.
For example, patients with uveitic glaucoma may not be ideal candidates because of the risk of worsening inflammation.
On the other hand, patients with a condition called plateau iris syndrome may actually benefit from the procedure because it causes the ciliary processes to shrink and potentially open up the angle of the eye.
The “angle” referred to here is the angle between the iris, which makes up the colored part of your eye, and the cornea, which is the outer, transparent structure at the front of the eye. The angle is the location where the aqueous humor (the fluid that is produced inside the eye) drains out of the eye into the body’s circulatory system.
As with any surgery your ophthalmologist recommends, a good question to ask is, “Why are you recommending this procedure specifically for my eye?”
What Results Should You Expect from Cyclophotocoagulation?
Whichever form of cyclophotocoagulation is chosen by your doctor, eye pressure lowering is the goal. Many studies have focused on patients with glaucomas that are difficult to control or treat. In general, however, a good rule of thumb is that the eye pressure generally decreases by 20 to 30 percent.
As mentioned earlier, because the ciliary processes can regenerate, sometimes the treatment needs to be repeated. In addition, sometimes the results of the treatment can be incomplete, even on purpose, since one of the risks of the procedure is a condition called hypotony, which is when the eye pressure becomes too low. Thus, some surgeons will elect to only partially treat the ciliary processes and stage the procedure over several sessions.
Common Risks of Cyclophotocoagulation
Common risks of cyclophotocoagulation include inflammation, which can cause the front of the eye to show signs of inflammation, or less commonly, the retina to swell (macular edema). Other more common risks include bleeding, especially in patients with a form of glaucoma called neovascular glaucoma. Less common side effects include vision loss, hypotony (described above), and a condition called sympathetic ophthalmia. In sympathetic ophthalmia, which is very rare, the untreated eye can begin “sympathizing” with the treated eye and become inflamed. Sympathetic ophthalmia is a treatable condition, but of course, because it involves the untreated eye, ophthalmologists are very careful with this laser procedure.
Summary
In summary, cyclophotocoagulation is a laser procedure that helps lower the eye pressure by targeting the part of the eye that produces fluid (ciliary processes). It can be very effective at lowering eye pressure, and the newer techniques are less invasive than traditional cyclophotocoagulation. However, even with the more traditional technique, surgeons may modify the laser settings to achieve the desired effect with less inflammation. It is best to discuss with your surgeon the various options available to you.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Glaucoma Surgery