Learn about uveitis: symptoms associated with this eye condition, treatment options, and how it is related to glaucoma.
What is Uveitis?
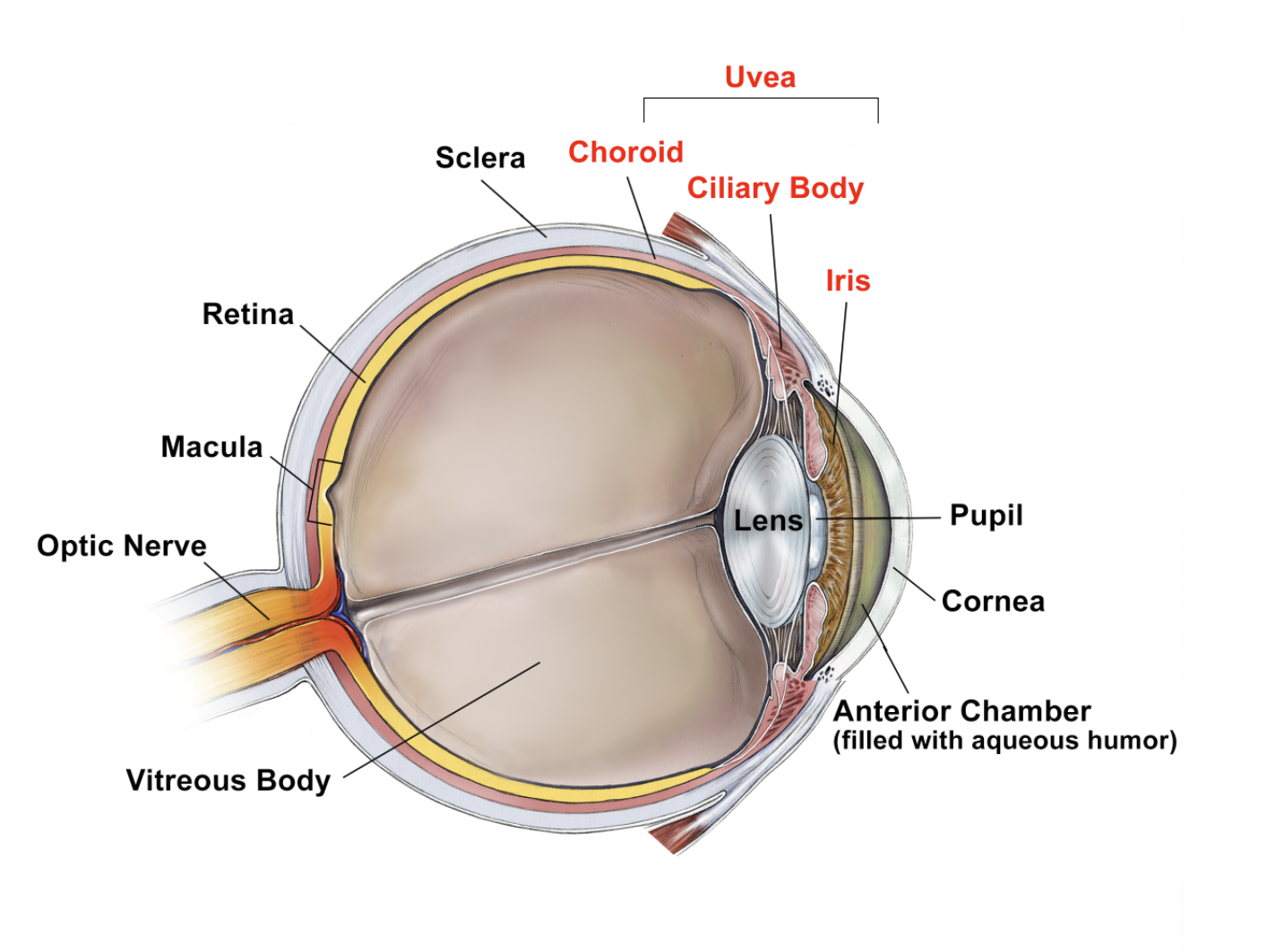
Uveitis is an eye condition that can lead to glaucoma. It is an inflammation of the eye, and typically affects the middle layer of the eye wall, which is called the uvea. The uvea is consists of iris, ciliary body, and choroid. The type of uveitis you have is determined by which parts of the eye are affected.
Video: Uveitis
Symptoms of Uveitis
The most common symptoms of uveitis are eye redness, pain, light sensitivity, floaters, and blurry vision. It can affect one eye or both eyes, and while it typically affects young to middle-aged adults, it can also affect children. Some causes of uveitis include infection, trauma, or an autoimmune disease, but many times, no cause is identified despite comprehensive testing.
Forms of Uveitis
Uveitis comes in many forms, depending on which part of the eye is affected. The most common type is iritis, also called anterior uveitis, and affects the front of the eye. Cyclitis, also called intermediate uveitis, affects the ciliary body. Choroiditis and retinitis, also called posterior uveitis, affect the back of your eye where the choroid and retina are. Panuveitis occurs when all of these layers exhibit inflammation.
Uveitis and Glaucoma
Glaucoma is thought to be a relatively common complication of uveitis, especially anterior uveitis and when the uveitis is more chronic and longstanding. It can occur through a variety of mechanisms. For example, steroids are most commonly used in the treatment of uveitis, but the steroids themselves can raise eye pressure, sometimes dramatically so. Other mechanisms include mechanical blockage of the drainage system of the eye by inflammatory cells. In chronic forms of uveitis, scar tissue can form over the drainage system of the eye from the inflammation and this can also lead to elevated eye pressure.
Treatment of Uveitis
The goal of uveitis treatment is to control the inflammation. The most common form of uveitis treatment is the use of steroids, with steroid eye drops as the most common initial form of treatment. In addition, treatments can involve the use of steroids injected in or around the eye and/or oral steroids in pill form. Also, there are medications that are called “steroid-sparing” and may modulate the immune system. If the cause of the inflammation is an infection, medications to treat the infection will be used. Finally, if the underlying cause of inflammation is a health issue that affects the entire body, such as autoimmune disease, that also needs to be treated.
It is important to understand that a treatment plan for uveitic glaucoma is multi-faceted. It involves treatment of the uveitis, treatment of glaucoma by lowering the eye pressure, and prevention of secondary effects from the uveitis that can lead to increased eye pressure. In complicated situations, a team approach involving a uveitis specialist, a comprehensive or glaucoma specialist, and a rheumatologist is important.
For the glaucoma treatment, some of the same medications and surgeries used for the most common type of glaucoma (primary open angle glaucoma) are also used to lower eye pressure in uveitic glaucoma. However, there are some nuances and the decision about which medications or surgeries to employ depends on the cause of the uveitis and whether it is in the acute phase or controlled phase. For example, laser surgery to lower eye pressure is not typically used for uveitic glaucoma because it can increase inflammation and potentially scarring.
Summary
In summary, there can be a connection between uveitis and glaucoma, although having uveitis does not necessarily mean you will develop glaucoma. Certainly, if you are under the care of an ophthalmologist for uveitis, he or she can determine whether you are showing any signs of early glaucoma or changes in the eye such as scarring in the drainage system. If caught early, glaucoma damage can be controlled or slowed so that it does not impact your vision.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.









