Learn what choroidal neovascularization is, why it occurs, how it is diagnosed, and options for treatment.
Some patients with dry age-related macular degeneration (AMD) eventually develop wet AMD, in which abnormal blood vessels grow into the retina and leak fluid, making the retina “wet.” Technically, this is called CNV or choroidal (core-oyd-al) neovascularization (nee-oh-vas-kyoo-lar-eye-zay-shun).
What Does Choroidal Neovascularization Mean?
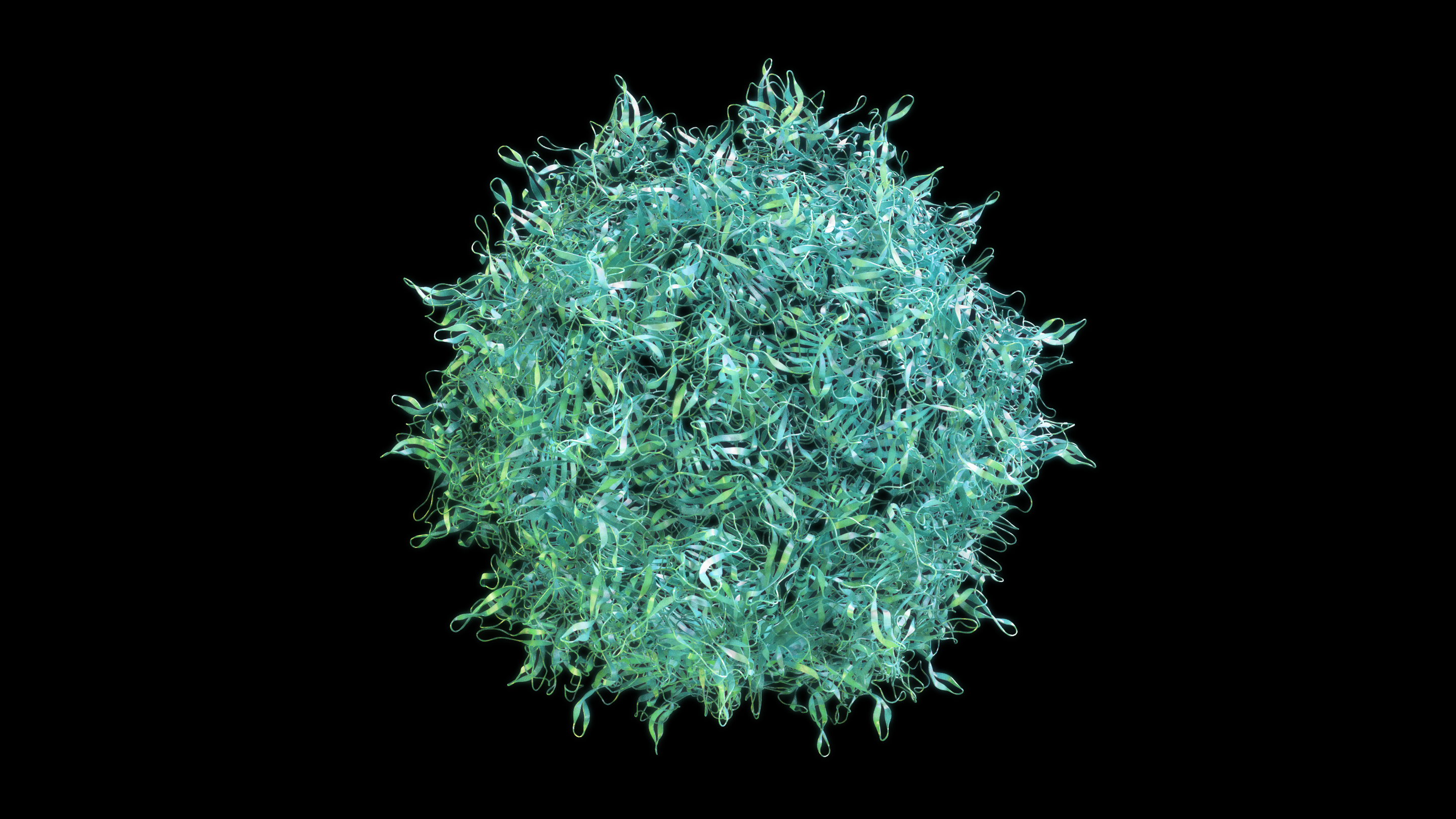
“Neovascularization” means “new blood vessels.” These new, abnormal blood vessels originate in the choroid, a vessel-containing layer under the retina. When the retinas of people with AMD produce too much vascular endothelial growth factor (VEGF), new blood vessels sprout from the choroid, then grow into the retina. The new vessels, unlike normal ones, are leaky, and they allow fluid from the blood, and sometimes even red blood cells, to enter the retina. This fluid can immediately distort the vision because it forms a “blister” in the retina, which is normally flat. Over the course of days to months, this fluid can damage the retina, killing the light-sensing cells, called photoreceptors.
Symptoms of Choroidal Neovascularization
The symptoms of CNV include a distortion or waviness of central vision or a gray/black/void spot in the central vision. This should prompt a call to an ophthalmologist right away to get a priority emergency visit. The ophthalmologist can halt the growth and leakage of the blood vessels by injecting a drug blocking a protein called VEGF into the eye, but only if they can deliver the drug as soon as possible, within hours or days or so from the time you notice the change in vision. Time lost is vision lost!
Diagnosing Choroidal Neovascularization
The ophthalmologist can detect CNV using a combination of techniques. First, during the dilated eye exam, she/he may see a blister of fluid or bleeding in the retina. Then, using specialized imaging called optical coherence tomography (OCT), a cross-section picture of the retina is obtained. This image can detect even small amounts of fluid that have leaked into the retina from CNV.
Additional imaging techniques called fluorescein or ICG angiography involve injection of a dye into a vein somewhere else in your body (where the dye gradually diffuses into the vessels in the back of the eye), followed by retinal imaging that shows the dye leaking from the blood vessels into the retina. These images sometimes provide additional information about the CNV.
Other Conditions That May Cause Choroidal Neovascularization
Age-related macular degeneration is the most common disease causing CNV, but other diseases that “stress” the retina, causing it to produce excess VEGF, or disrupting the barrier between the retina and choroid, can also cause CNV.
- In patients with pathologic myopia (extreme nearsightedness), the eye is longer than normal, and this lengthening stretches and stresses the retina.
- Ocular histoplasmosis is a fungal infection that can cause CNV.
- Eye trauma and angioid streaks (small breaks in one of the retina’s layers) can break the barrier between the retina and choroid, resulting in CNV.
- Severe ocular inflammation, a condition called uveitis, can also cause CNV.
Treatment of Choroidal Neovascularization
Most patients with these diseases benefit from injection into the eye of anti-VEGF drugs, such as brolucizumab (Beovu®), aflibercept (Eylea®), or ranibizumab (Lucentis®), since VEGF promotes the CNV growth and leakage in most cases.
New research is bringing longer lasting anti-VEGF drugs, like brolucizumab, and anti-VEGF gene therapy, which should enable the anti-VEGF effect to last longer, so patients will not need to have injections as frequently.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Disease Biology
- Wet AMD