
Iridocorneal endothelial syndrome, or ICE syndrome, is a group of eye diseases that can lead to glaucoma.
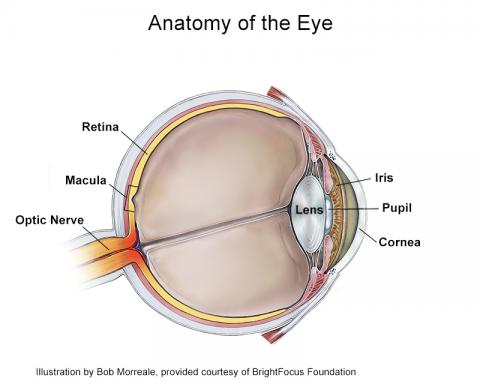
In order to understand why ICE syndrome can lead to glaucoma, it is important to understand eye anatomy in some detail.
The features of ICE syndrome include:
- swelling of the cornea, or the clear front part of the eye,
- abnormalities of the iris, the colored part of the eye that contains the pupil, and
- a high risk of developing glaucoma.
The cornea, or clear front part of the eye, is an important part of the eye as it not only protects the eye but also maintains its clarity for it to properly focus light. The cornea is made up of many layers, the innermost layer being composed of endothelial cells. These endothelial cells play an essential role in keeping the cornea clear, as they pump out fluid from the cornea and keep it compact and clear.
The iris, or colored part of the eye that forms the pupil, also plays an important role in controlling the amount of light that enters the eye, much like the way a camera has a small aperture or opening to allow light through.
A normal iris will dilate in darkness and constrict to light (and also when we focus on something that is close, such as a book that we are reading).
In ICE syndrome, the endothelial cells that line the innermost part of the cornea are abnormal, and they do not perform their role in keeping the cornea clear, and the cornea can become cloudy.
These abnormal cells can also increase in number and migrate to areas where they do not belong. One of these areas is the drainage system of the eye, which is near the edge of the cornea. The abnormal endothelial cells migrate across the drainage system and can cause the eye pressure to build up. In addition, the abnormal cells can migrate onto the iris and cause the pupil to be misshapen, or sometimes even cause the iris to stretch so much that holes form.
In another form of ICE syndrome, the abnormal cells can migrate onto the iris and cause clumping of little islands of iris tissue and form small nodules, sometimes called Cogan-Reese nodules.
You may hear your ophthalmologist describe ICE syndrome as:
- Chandler syndrome (where the main abnormality is in the cornea)
- Essential iris atrophy (where the abnormal cells cause the iris to stretch and form holes), or
- Iris Nevus / Cogan-Reese (characterized by iris nodules described above).
All these forms of ICE syndrome have abnormal corneal endothelial cells and are associated with increased risk of glaucoma.
ICE syndrome usually affects women more often than men, most commonly diagnosed between the ages of 30-50. It is usually in one eye, although it can affect both eyes.
Diagnosis
Chandler syndrome is probably the most common form of ICE syndrome, but it is also the most difficult to diagnose because the changes in the eye can be more subtle. One test that can help an ophthalmologist make the diagnosis is specular or confocal microscopy. In this test the corneal endothelial cells are imaged, and their shape, size or number will be abnormal. Other tests include ones that are normally performed during a glaucoma evaluation, such as gonioscopy (an examination of your drainage angle using a special mirrored lens), eye pressure and corneal thickness measurements, visual field testing, and optic nerve imaging.
Secondary Angle-Closure Glaucoma
So how does ICE syndrome cause secondary angle-closure glaucoma? The most likely answer is that the abnormal endothelial cells grow and migrate over the trabecular meshwork, the internal drainage system of the eye. The cells can also cause the iris tissue to contract and further block the drainage angle.
Treatment
Medication
ICE syndrome-associated glaucoma is typically first treated with medications, which help lower eye pressure. One consideration your ophthalmologist may raise is whether medications such as latanoprost should be used. This is because latanoprost can reactivate herpes simplex virus, which may be a potential cause of ICE syndrome. However, a definitive cause has not yet been identified.
Tube Shunt Surgery
Glaucoma drainage device or tube shunt surgery is worth considering because the tube can be placed far away from the drainage angle, thereby preventing the abnormal cells from migrating over the opening.
Corneal Transplant
Finally, if the cornea swelling is impeding vision, a partial or full corneal transplant can be a good solution and is often more successful if eye pressure is first controlled with medications and/or surgery.
Treatment Concerns
Considerations in treating ICE syndrome include the avoidance of the use of laser trabeculoplasty, which generally does not help improve outflow because of the abnormal cells growing over the trabecular meshwork.
Some of the newer MIGS (minimally invasive glaucoma surgeries) are also not ideal procedures because the abnormal cells can grow over the small tube openings, such as the iStent® or CyPass®*.
Traditional filtering surgeries such as trabeculectomy are successful in the short term, but over time the small hole that is created during the surgery can also be blocked by the abnormally migrating endothelial cells.
Summary
While glaucoma associated with ICE syndrome can be challenging to treat, seeking appropriate care with a glaucoma specialist you trust will help to provide the best outcome for your vision.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Risk Factors









