What Can Down Syndrome Tell Us About Alzheimer's Disease and Aging?
Written by BrightFocus Contributors Aurélie Ledreux, PhD & Lotta Granholm-Bentley, PhD/DDS, Department of Neurosurgery at the University of Colorado Anschutz Medical Campus
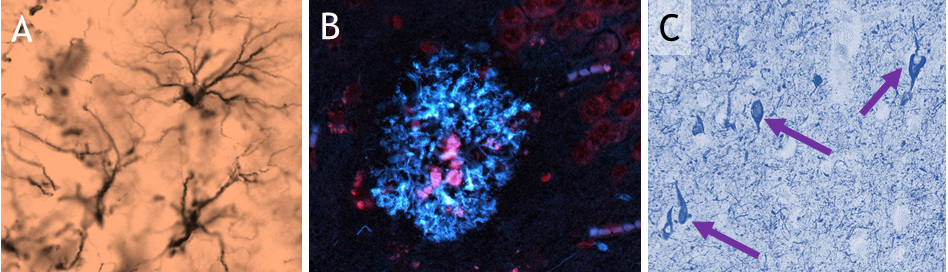
Dr. Granholm-Bentley received a 2017-23 Alzheimer’s Disease Research grant from BrightFocus to create the International Brain Bank for Down Syndrome-Related Alzheimer’s Disease, a collaborative research network focused on developing and sharing high-quality biological research samples and studying much-needed information about the Down syndrome population. Up to 80 percent of all Down syndrome individuals develop Alzheimer’s by the time they are in their 50s and 60s, and the project is exploring the neurobiological mechanisms underlying the onset of Alzheimer’s disease-type dementia in Down syndrome, as well as possible treatment targets for this population. Co-principal investigators on the grant include Elizabeth Head, PhD, of the University of California, Irvine; and Elliott Mufson, PhD, of the Barrow Neurological Institute.