Breaking News Dispatch: New Findings on GLP-1 Drugs and Alzheimer's, Novel Treatments in Development, and More
Get the latest news from the 2025 Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Get the latest news from the 2025 Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Leaders in Alzheimer’s research shared the latest advancements transforming Alzheimer’s diagnosis and treatment at the Clinical Trials on Alzheimer’s Disease (CTAD) conference last week in San Diego.
Explore the top headlines, including results from a first-of-its-kind clinical trial testing the GLP-1 drug semaglutide’s effect on Alzheimer’s disease, a novel tau-targeting therapy, and new blood tests (biomarkers) that could help detect Alzheimer’s earlier.

Results from the EVOKE trials, the largest clinical study to date with the GLP-1 drug semaglutide in Alzheimer’s disease, showed that semaglutide did not significantly slow disease progression in people with early-stage Alzheimer’s.
The drug tested was Rybelsus, a pill approved for type 2 diabetes manufactured by Novo Nordisk. While treatment with semaglutide did not delay disease progression, treatment did improve some Alzheimer’s disease-related biomarkers, such as different forms of tau protein and markers of brain inflammation and nerve cell damage.
GLP-1 drugs still show promise for addressing mid- and late-life modifiable risk factors to prevent or delay the onset of Alzheimer’s disease. These include helping to maintain target blood sugar levels and a healthy metabolism, said Sharyn Rossi, PhD, BrightFocus Foundation’s senior director of neuroscience programs.
Research continues into other GLP-1-based drugs to assess their potential impact on Alzheimer’s disease.
“While semaglutide did not demonstrate efficacy in slowing the progression of Alzheimer’s disease, the extensive body of evidence supporting semaglutide continues to provide benefits for individuals with type 2 diabetes, obesity, and related comorbidities,” Martin Holst Lange, chief scientific officer and executive vice president of research and development at Novo Nordisk, said in a statement.

The U.S. POINTER study showed that a structured healthy lifestyle program can protect cognitive function in adults at risk for cognitive decline. New follow-on data from three ancillary studies reveal additional benefits: improved blood pressure, reduced sleep apnea, and greater cognitive resilience—the brain’s ability to maintain function despite the presence of Alzheimer’s-related brain pathology.
The program focused on four lifestyle areas: physical activity, the MIND diet, cognitive challenge, and health monitoring.
“We are excited about this finding, as it shows that the structured intervention improves not only cognition but also other behaviors that affect brain health, which may increase protection against dementia,” said Laura D. Baker, PhD, Professor, Internal Medicine and Public Health Sciences and Associate Director, Wake Forest Alzheimer’s Disease Research Center at the Wake Forest University School of Medicine. “The positive effect of the structured intervention on sleep deepens the significance of the U.S. POINTER trial results for older Americans.” Dr. Baker is one of the principal investigators of the parent trial and principal investigator of the sleep ancillary study.
Watch our conversation with Dr. Baker about the U.S. POINTER trial, the largest study of its kind to test how lifestyle changes impact brain health.
Merck presented first-in-human data for two novel therapies in Phase 2 clinical trials. The first, MK-2214, targets the abnormal accumulation and aggregation of tau in the brain and has been granted Fast Track Designation by the U.S. Food and Drug Administration. Fast Track is designed to facilitate the development and expedite the review of drug candidates to treat serious conditions and address an unmet medical need. There are currently no FDA-approved disease-modifying therapies that target tau, which, along with amyloid-beta, is a hallmark protein of Alzheimer’s disease.
The second therapy, MK-1167, is an investigational oral treatment that is taken along with donepezil, an approved acetylcholineraste inhibitor, to improve symptoms of Alzheimer’s. In a Phase 1 first-in-human study, MK-1167 increased glutamate metabolism in the brain’s prefrontal cortex, crucial for cognitive functions like decision-making, memory, and emotional regulation.

Drug developer Alzheon presented new safety and efficacy data for Valiltramiprosate/ALZ-801, an oral treatment for people with a high genetic risk for Alzheimer’s. The results from the Phase 2 study long-term extension over 3 years showed clinically meaningful and significant effects on slowing both cognitive and functional decline and preserved brain volume in individuals with mild cognitive impairment and two copies of the APOE4 gene—a group that is often unable to take currently available Alzheimer’s drugs due to safety concerns. This is the first interventional Alzheimer’s drug trial focused on high-risk APOE4/4 individuals.
“Positive clinical and structural brain outcomes from the APOLLOE4 Phase 3 program continue to strengthen the case for valiltramiprosate as a potential breakthrough oral treatment for the high-risk APOE4 population,” said David Watson, PhD, founder & principal investigator, Alzheimer’s & Research Treatment Center in a statement. “Therapies that safely reduce the formation of toxic amyloid oligomers at the start of the disease process have the potential to shift how and when we treat Alzheimer’s disease. ALZ-801 has shown that promise in clinical trials.”

Scientists presented new clinical data highlighting circular RNAs (circRNAs), a novel, noninvasive blood biomarker platform for early detection of Alzheimer’s disease. This approach, supported by funding from Alzheimer’s Disease Research, offers scientists a more comprehensive view of the many biological changes that happen in Alzheimer’s disease.
More accurate biomarkers are key to earlier intervention and treatment. By providing an accurate, accessible, and specific molecular assessment of the disease, physicians can better identify people with Alzheimer’s early in the disease process—even before symptoms appear—ultimately leading to more timely interventions, the company stated.
At CTAD, Dr. Carlos Cruchaga, a member of BrightFocus Foundation’s Alzheimer’s Disease Research Scientific Review Committee, and grantee Laura Ibañez, PhD, presented data on the circRNA biomarker model that could more accurately identify and diagnose Alzheimer’s in the blood. These findings are being licensed by Circular Genomics, which is developing clinical assays (lab tests) that could reshape the standard of care for the early identification of neurological and psychiatric diseases like Alzheimer’s.
“We have successfully identified a robust blood circRNA biomarker signature that is best-in-class at detecting Alzheimer’s biology and pathology across the entire disease continuum representing a transformative pathway to significant improvements over existing standard-of-care methods,” said Nikolaos Mellios, MD, PhD, chief scientific officer and co-founder of Circular Genomics in a statement. “Circular RNAs are brain-derived, highly stable, and measurable biomarkers in blood, providing an unprecedented, real-time window into brain health. This precision neurology approach, leveraging the unique insights from circRNA, is critical to facilitating early diagnosis and treatment for Alzheimer’s.”
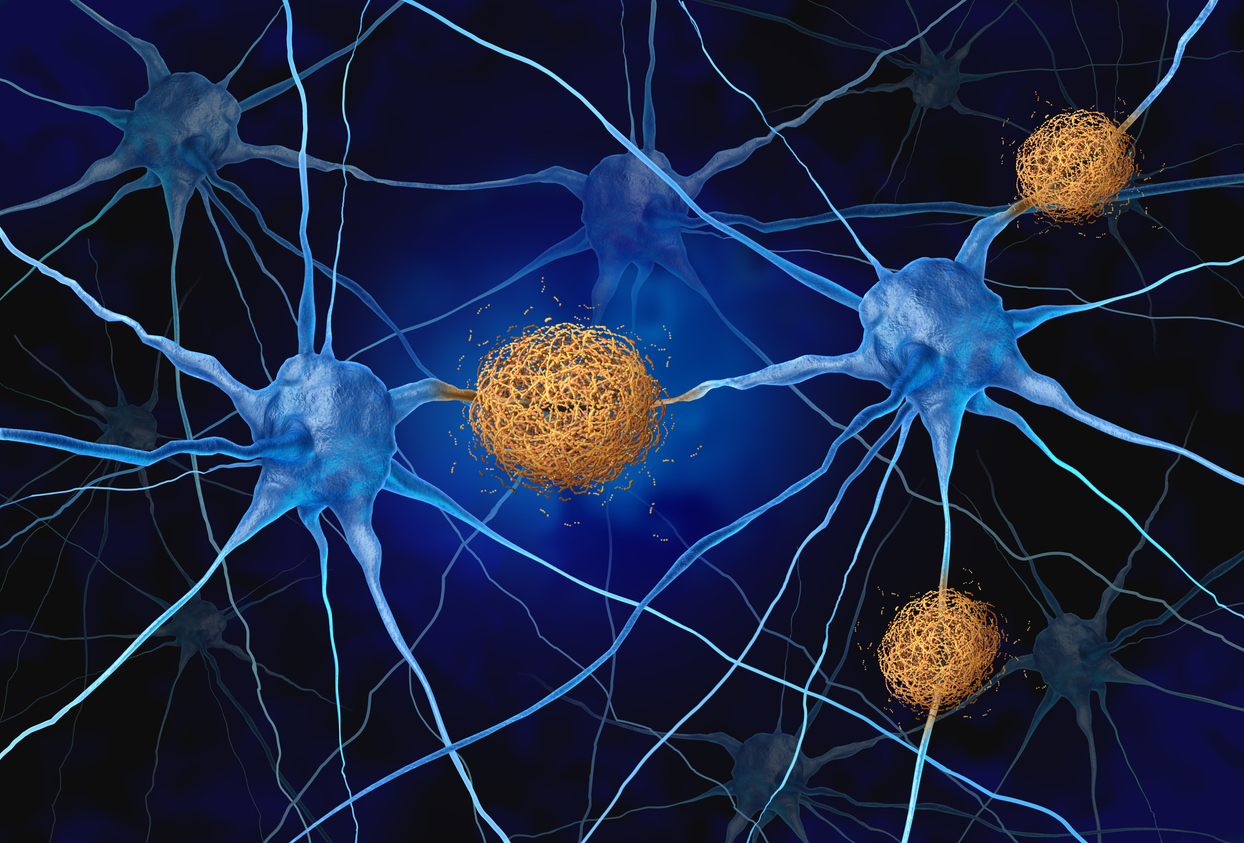
Trontinemab, a disease-modifying drug designed to rapidly clear amyloid plaques from the brain, is moving ahead into Phase III trials. The drug uses Roche’s proprietary Brainshuttle technology to enhance drug delivery across the blood-brain barrier. Results are expected in 2028, after which Roche can pursue regulatory approval if the findings are positive.
In its Phase I/II Brainshuttle AD study, 92% of people receiving trontinemab showed no measurable amyloid plaques after 28 weeks of treatment. There was a low incidence of amyloid-related imaging abnormalities (ARIA), indicative of swelling or bleeding in the brain. Two identical Phase III studies, TRONTIER 1 and 2, are underway to evaluate the efficacy and safety in people with early symptomatic Alzheimer’s disease.
Learn more about trontinemab and other emerging Alzheimer’s therapeutics in late-stage clinical development.
The future of Alzheimer’s treatment may lie in intervening before symptoms appear. For example, the AHEAD study is testing whether early treatment with Leqembi (lecanemab) can slow or stop brain changes associated with Alzheimer’s disease in people at higher risk before memory loss begins. Lilly is evaluating Kisunla (donanemab) in people with preclinical Alzheimer’s, and Roche plans to study trontinemab in this early stage as well. With advances in blood biomarkers enabling earlier detection, researchers hope to ultimately delay—or even prevent—the onset of this disease.
Learn more about the AHEAD study on December 18 during an episode of Zoom In on Dementia & Alzheimer’s with Dr. Joshua Grill.
Alzheimer’s Disease Research grant recipient Gemma Salvadó, PhD, presented findings on a groundbreaking blood test that could identify and predict early amyloid accumulation in cognitively unimpaired individuals. This could enable earlier intervention and treatment, even before symptoms begin. Learn more about her work.
Biotech company CervoMed presented new data indicating that its oral neflamapimod treatment for dementia with Lewy bodies led to a significant reduction in widely used neurodegeneration biomarkers, including plasma glial fibrillary acidic protein and beta amyloid 42/40 ratio. Lewy body dementia is the second most common form of dementia with no approved treatments.
View Alzheimer’s disease resources and learn more about the innovative research funded by BrightFocus Foundation’s Alzheimer’s Disease Research program.
Did you miss our previous Breaking News Dispatches from top Alzheimer’s and dementia conferences? Catch up here.
This Breaking News Dispatch is supported by sponsorship funding from Lilly.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
Every Donation is a Step Forward in the Fight Against Alzheimer’s
Your donation powers cutting-edge research and helps scientists explore new treatments. Help bring us closer to a cure and provide valuable information to the public.
Donate Today