Macular pucker (also known as an epiretinal membrane) is an eye condition that affects the central retina, or macula. As the name suggests, it is caused by distortion or “squeezing” of the macula. The condition is sometimes called “cellophane maculopathy,” because it can be caused by a thin, transparent layer of cellophane-like scar tissue tugging on the neurons of the macula.
While macular pucker is a different disease than age-related macular degeneration, the two diseases can have similar symptoms, such as wavy or distorted vision in the center of the visual field. Macular pucker usually causes only mild distortion of vision in one eye; however, less often it can affect both eyes and can cause significant loss of central vision.
The scar tissue is stimulated to grow by injury to the eye. The most common type of “injury” is the separation of the jelly (vitreous) in the center of the eye from the retina, which occurs in most people during the aging process. The vitreous is made of water and a network of tiny fibers. When these fibers separate from the retina, they tug on it and this can cause enough damage to stimulate growth of scar tissue. Alternatively, the scar tissue growth may be stimulated by inflammation in the eye, trauma, and perhaps, rarely, cataract surgery.
Video: What Is Macular Pucker?
Diagnosis and Monitoring Macular Pucker
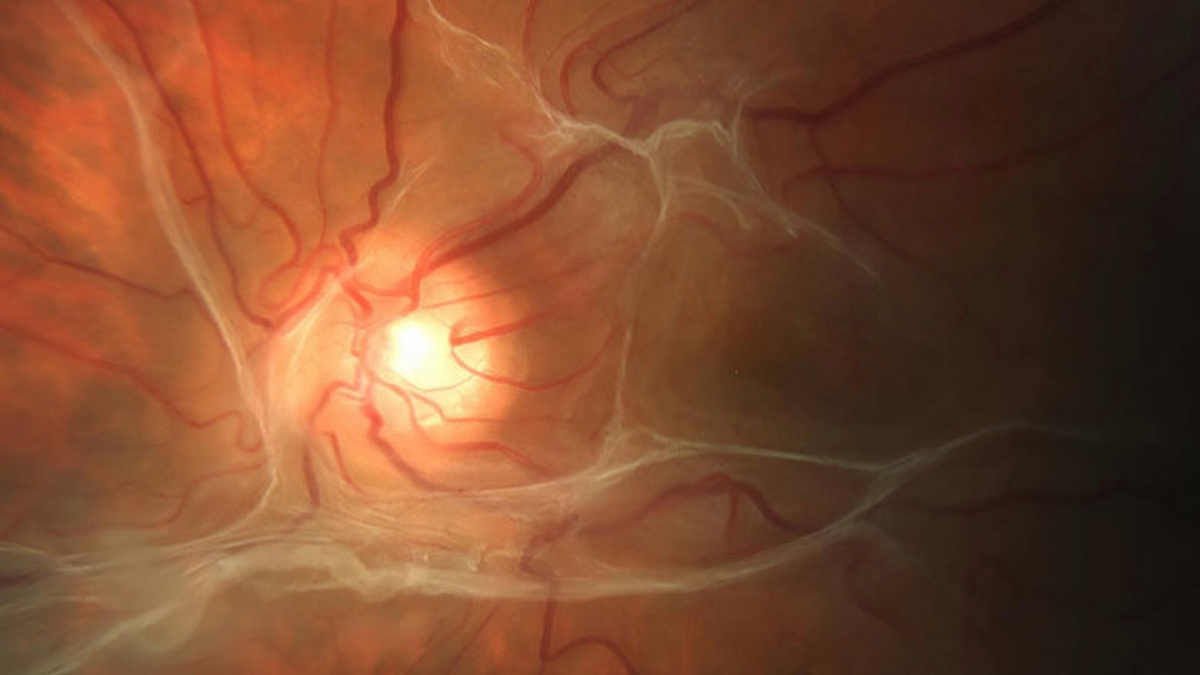
Macular pucker can be diagnosed by an ophthalmologist performing a retinal examination following pupil dilating drops. Its progress can be followed over time by measuring visual acuity, checking for distorted vision while looking at a graph called an Amsler grid, or by special photographs. These can include color photographs of the retinas, and important cross-section photos of the retina taken by a process called optical coherence tomography (OCT). The OCT shows the extent of retinal scar formation and retinal distortion caused by traction from the scar tissue.
Treatment: Non-Surgical Interventions Macular Pucker
Since most patients have only mild symptoms, they can best benefit from new glasses, reading lamps, and perhaps magnifiers. For patients with more severe symptoms, medical or surgical treatment may be appropriate. A subgroup of patients with macular pucker that is caused by the vitreous tugging on the macula (vitreomacular traction) may benefit with a single injection into the eye of a medication called Jetrea. This drug is an enzyme that digests the tiny fibers in the vitreous, potentially releasing the traction.
Treatment: Macular Pucker Surgery to Remove Scar Tissue
For patients who would not benefit from Jetrea, surgery may be helpful. The outpatient surgery is done with local anesthesia and involves removing the vitreous (vitrectomy) and usually peeling off the cellophane-like scar tissue. This can help relieve the retinal traction, decreasing distortion of the vision, and improving visual acuity.
Related Disorders
A related disease is the macular hole, which can result from traction on the retina, and can also require vitrectomy surgery to relieve the traction and close the hole. Another disease, retinal detachment, occurs when the retina separates from the back of the eye, usually caused by a tear in the peripheral retina resulting from the vitreous tugging on the retina as it separates. The symptoms of a retinal tear/detachment in one eye are:
- Arcs of flashing light in the peripheral vision;
- New floating black dots in the vision; or
- A curtain blocking the peripheral vision, which may enlarge to block the central vision.
Since a retinal tear is an emergency, patients with the symptoms of a retinal tear/detachment should call their ophthalmologist immediately to receive vision-protecting treatment if a tear or detachment is diagnosed.
Retinal Detachment Video
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Disease Biology









