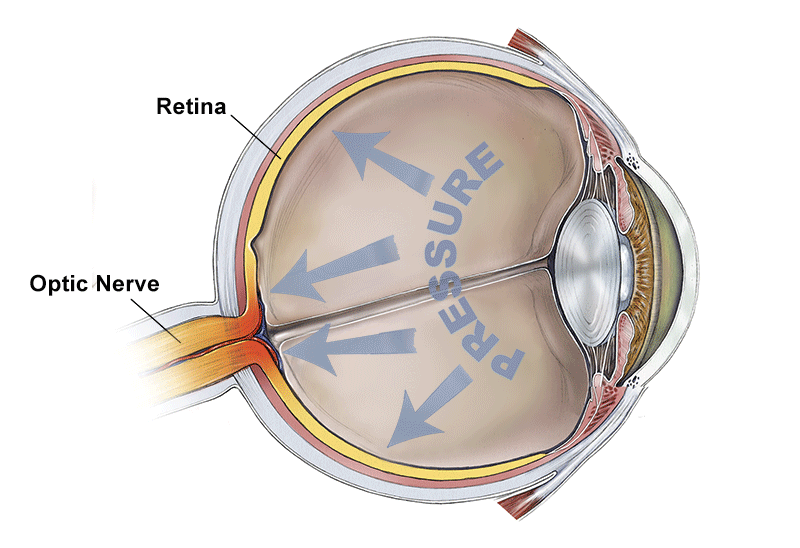
Ocular hypertension is a condition in which the measured eye pressure (intraocular pressure or IOP) is consistently greater than “normal.” However, there is no obvious damage to the optic nerve as detected by an eye examination, optic nerve imaging, or evidence of visual field change. In other words, there is no evidence of glaucoma yet.
In considering what constitutes ocular hypertension, it is important to recognize that “normal” eye pressure likely depends on many different factors, including age and ethnicity, as well as factors such as corneal thickness (more on that below).
In the United States, the prevalence of ocular hypertension in non-Hispanic Whites who are 40 years of age and older is 4.5 percent, and increases up to 7.7 percent in 75 to 79 year olds. In Latinos, the prevalence across ages is quite similar. Because ocular hypertension occurs typically without symptoms, a majority of people with ocular hypertension remains undiagnosed. In the Los Angeles Latino Eye Study, 75 percent of Latinos with eye pressures greater than 21 mmHg were previously undiagnosed.
Video: Ocular Hypertension
Why is Ocular Hypertension Important?
Eye pressure is one of the major risk factors for the development of glaucoma. That being said, there are also plenty of individuals who never demonstrate elevated eye pressure but do have glaucoma. This is called “normal-tension” or “low-tension” glaucoma.
What are the Risk Factors?
It is estimated that three to six million persons in the United States have ocular hypertension. These are individuals whom an eye care provider will follow closely for the development of glaucoma. The likelihood of developing glaucoma increases with the number and relative strength of risk factors.
Risk factors of ocular hypertension include:
- higher eye pressure,
- older age,
- family history of glaucoma,
- lower ocular perfusion pressure (this is related to blood pressure and eye pressure),
- lower systemic blood pressure,
- thinner central cornea, and
- bleeding at the optic nerve head.
Corneal Thickness
Central corneal thickness is an independent risk factor for the development of glaucoma. The cornea is the clear “window” of the eye and whenever eye pressure is measured, the biomechanical properties of the cornea play a role in the accuracy of the measurement.
When using applanation tonometry (one of the most common forms of eye pressure measurement), eye pressure may be overestimated with thicker corneas and underestimated with thinner corneas. There has been a lot of research trying to establish the exact relationship between eye pressure as measured by various techniques and central corneal thickness, but there is no widely accepted formula to account for an individual’s central corneal thickness. However, most eye care providers would take into consideration central corneal thickness. For example, a patient with thin corneas and high eye pressure would be considered higher risk than a patient with thick corneas and high eye pressure.
Low Blood Pressure
It is interesting to note that while higher blood pressure can indeed raise eye pressure by a very small amount, lower blood pressure is actually a risk factor for the development of glaucoma. This is likely due to the fact that lower blood pressure means lower perfusion pressure and decreased blood flow to the eye and optic nerve, which is a risk factor for the development of glaucoma.
How Quickly Can Ocular Hypertension Develop Into Glaucoma?
One well done and critical study that provided important information about ocular hypertension and the development of glaucoma is the Ocular Hypertension Treatment Study (OHTS). It demonstrated that the rate of untreated ocular hypertension patients in developing glaucoma was 9.5 percent in 5 years and 22 percent at 13 years, or about 2 percent per year. With treatment, the risk of developing glaucoma was reduced by about 50 percent.
When Should Treatment Begin?
So how do we decide whether a patient with ocular hypertension should be treated? This decision is complex, and should be undertaken together by both the patient and eye doctor. The eye doctor will consider the findings of the eye exam, risk factor assessment, testing such as optic nerve imaging and visual field testing and the patient’s preferences and ability to adhere to a treatment plan. The decision to begin treatment is particularly important in the case of ocular hypertension patients or glaucoma suspects, because treatment is long-term and exposes the patient to the side effects and costs of treatment. For some patients, the eye doctor and patient will reach the conclusion that the risk of developing glaucoma is high enough to justify treatment. The OHTS study provides some guidance on this topic as those with higher eye pressures and thinner corneas were most at risk for developing glaucoma.
There are also situations that are clearer with regard to when a patient with ocular hypertension should undergo treatment. Patients who demonstrate optic nerve damage or visual field changes over time should be treated because they have likely developed early glaucoma.
The bottom line is that a patient with ocular hypertension should have long-term follow-up with their eye doctor to monitor the potential development of glaucoma or to gauge the effectiveness of treatments that are implemented.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Disease Biology
- Eye Health
- Risk Factors









