Optic nerve imaging provides an objective test to diagnose and follow the progression of glaucoma, and the technology has undergone tremendous advancements over the last decade.
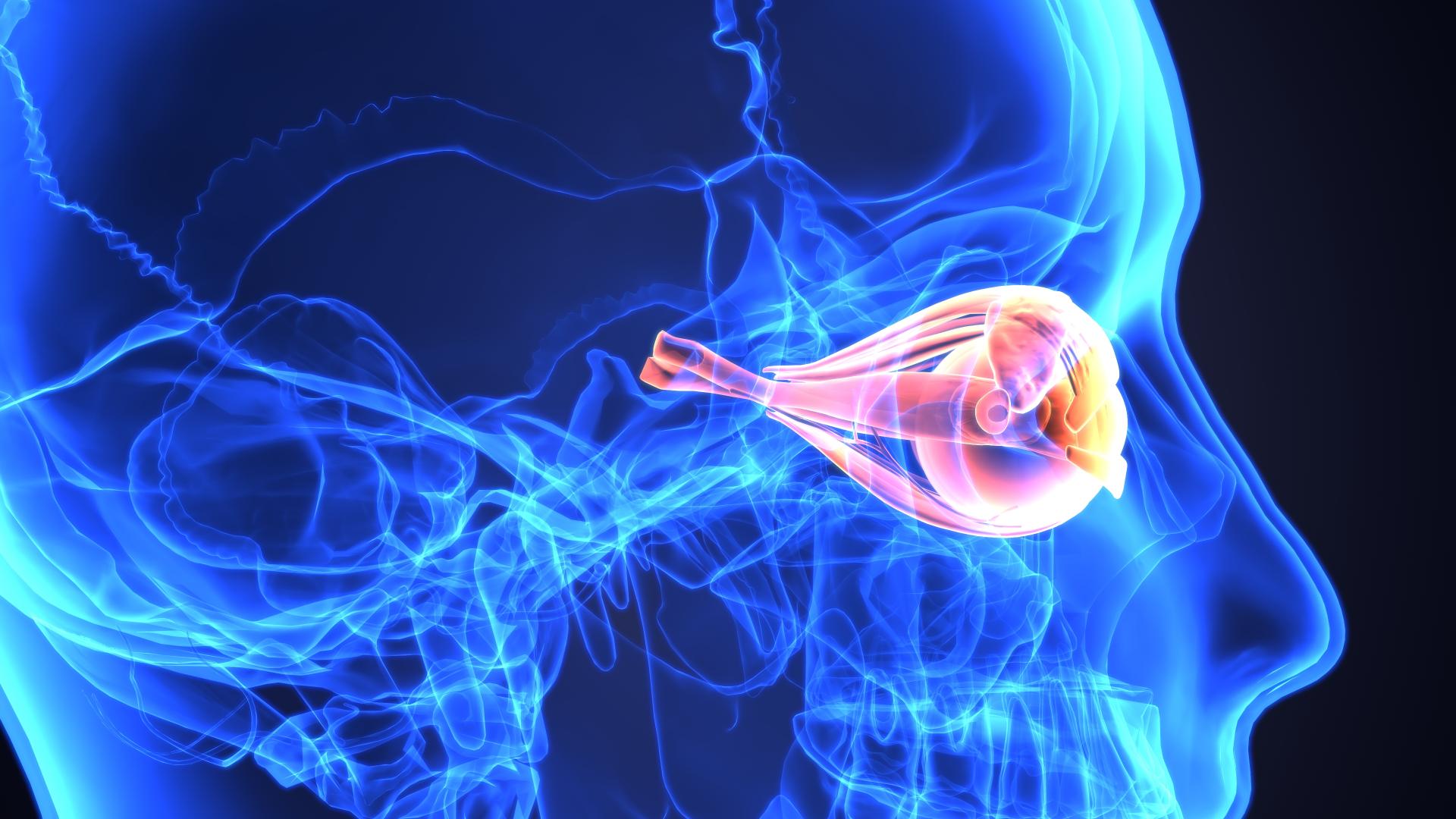
When an eye doctor evaluates a patient for glaucoma, one very critical aspect of the office visit is the careful examination of the optic nerve. The optic nerve is composed of approximately 1.5 million axons that connect the retina to the visual targets in the brain. Axons can be thought of as long “cables” or “extensions” of the retinal ganglion cells, which are the cells that are damaged in glaucoma. When the axons and the retinal ganglion cells are damaged, there is loss of function of the optic nerve, which results in visual field deficits. While the visual field tests are very important for glaucoma diagnosis and for tracking glaucoma over time, it is a subjective test. Factors such as alertness, noise or distractions in the surroundings, or how the test is setup can affect how well someone performs on a field of vision test. Therefore, it is very important to also have an objective test to diagnose and follow glaucoma, and the technology of optic nerve imaging has undergone rapid advancements over the last decade.
Optic Nerve Photographs
A very important type of optic nerve imaging involves optic nerve photographs, or stereo disc photography. These photographs are useful because they give detailed documentation of the appearance of the optic nerves, and they can be used as a baseline for future comparisons. Furthermore, a good set of color optic nerve photographs will be forever useful even as technology advances. Stereo disc photography allows the eye doctor to detect if there has been any change in the optic nerves since baseline photographs were taken. Taking a set of stereo disc photographs does require the eyes to be dilated and for the eye doctor to have specialized equipment. If you believe you have previously had optic nerve photographs taken, it is worth your effort to call the doctor’s office and obtain digital copies. This way if you move or change eye doctors, a review of your prior photographs can help the new provider determine if there has been progression or stability of your glaucoma.
Advanced Imaging Techniques
More recently, the introduction of more advanced optic nerve imaging techniques have allowed the quantification of certain parameters related to the optic nerves and retina. While optic nerve photographs provide an objective documentation of the appearance of the optic nerves, it does not provide quantitative information. This is one major advantage of the advanced techniques.

A young woman with glaucoma preparing to have an optic nerve imaging test using optical coherence tomography.
The next section lists some of the more common optic nerve imaging techniques. The goal of all of these techniques is to measure the thickness of the nerve fiber layer.
The nerve fiber layer is the part of the retina that contains the axons of the retinal ganglion cells. In glaucoma, there is thinning of the retinal nerve fiber layer. Thus, eye doctors can use it both for diagnosing glaucoma, as there are characteristic areas in which the retinal nerve fiber layer thins first, as well as for monitoring the stability of the disease over time. For example, the test can indicate whether the retinal nerve fiber layer thickness is stable on repeat examination, or if there is progressive thinning.
- Optical Coherence Tomography (OCT): OCT measures the reflection of laser light similar to the way that ultrasound measures the reflection of sound. Using this device, a 3D reconstruction of the optic nerve can be created. The most recent advances of OCT include OCT-A, or OCT-Angiography, whereby the blood flow to vessels surrounding the optic nerve and in the macula can be measured. This is still an active area of research, but we do know that some patients’ optic nerves are very vulnerable to changes in optic nerve blood flow, and this new measurement may be useful in evaluating these patients.
- Heidelberg Retina Tomograph (HRT): HRT is also a laser that can produce a 3D representation of the optic nerve.
- Nerve Fiber Analyzer (GDx): GDx uses laser light to measure the thickness of the nerve fiber layer.
There are nuances between the instruments, but they all serve the purpose to quantitatively analyze the nerve fiber layer thickness and measure certain parameters of the optic nerve head and macula. The lasers are all safe for the eye, and the test is quick and painless. During the test, the chin is placed on chin rest and the forehead presses against a bar, similar to a normal eye examination with an eye doctor. The technician or eye doctor tests each eye individually, and instructions are given with regard to where to focus and when it is all right to blink.
Video: Optical Coherence Tomography
Summary
In summary, optic nerve imaging is one of several tests and examination findings that an eye doctor will use to diagnose and monitor glaucoma. It is an important addition to eye care, and has the advantage of providing an eye doctor with objective data regarding the optic nerves and macula.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Eye Tests









