Hope for Strategically Breaching the Blood-Brain Barrier in Alzheimer’s Disease
Written By: BrightFocus Editorial Staff
Written By: BrightFocus Editorial Staff
What: An international team of researchers discovers a way to manipulate the permeability of the blood-brain barrier to treat neurological disorders, including Alzheimer’s, and let drugs enter the brain.
Where: Hashimoto et al. Claudin-5: A Pharmacological Target to Modify the Permeability of the Blood–Brain Barrier. Biological and Pharmaceutical Bulletin, 2021 (published by the Pharmaceutical Society of Japan).
BrightFocus Connection: The work was supported by an Alzheimer’s Disease Research (ADR) grant to Matthew Campbell, PhD, of Trinity College Dublin, whose lab focuses primarily on the vasculature associated with neural tissues. Dr. Campbell also is a past grantee of the Macular Degeneration Research program.
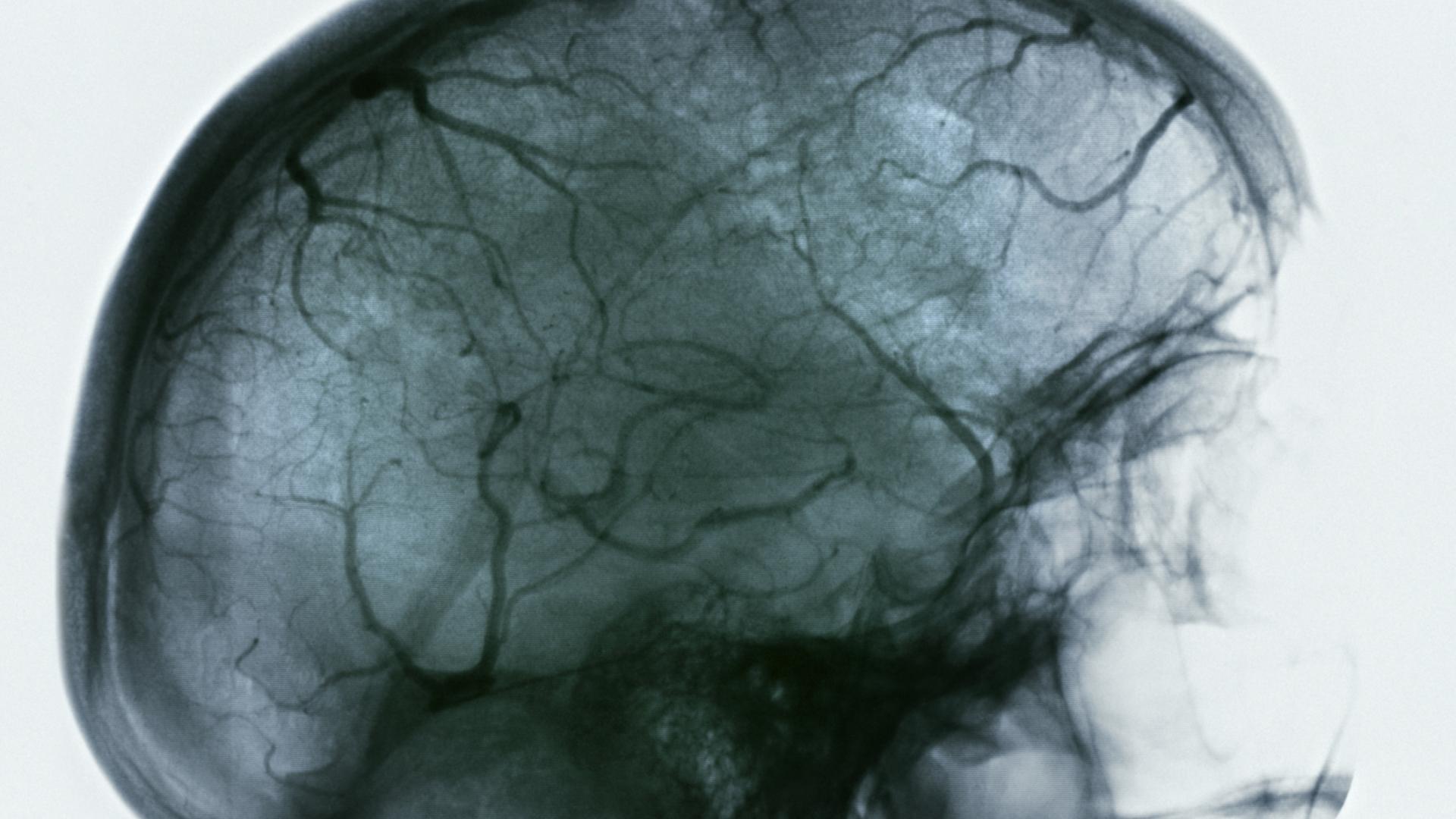
Why It Is Important: Blood vessels are lined with a type of cells called endothelial cells. In most tissues of the body, there are small spaces between endothelial cells that molecules can pass through, thus permitting passive two-way diffusion of particles in blood and tissue. In the brain, however, the endothelial cells lining blood vessels are tightly sealed with mesh-like structures known as “tight junctions” that form the blood-brain barrier (BBB), an essential defense against blood-borne pathogens entering the brain. The BBB poses a challenge to getting potentially helpful agents, like drugs, into the brain, and in certain situations, it may also prevent damaging materials, like the amyloid-ꞵ plaques that accumulate in the brains of people with Alzheimer’s, from getting cleared out of the brain.
The most prominent protein in tight junctions is claudin-5. Its structure prevents molecules within a certain size range from moving through the BBB. Hypothetically, drugs that increase claudin-5 expression diminish the permeability of the BBB and could be used to treat advanced central nervous system disorders in which the BBB becomes too porous, including Alzheimer’s, mood disorders, multiple sclerosis, and epilepsy. Conversely, drugs that thwart claudin-5 could increase BBB permeability and allow the passage of drugs into the brain.
Manipulating claudin-5 expression provides a size-specific, and therefore safer, way of interfering with the BBB than older methods that remove it completely. Dr. Campbell’s earlier work in mice showed that suppressing claudin-5 opened the BBB enough to allow toxic amyloid-ꞵ plaques to leave the brain. Fortunately, there are already approved drugs for mood disorders that enhance claudin-5, and some claudin-5 inhibitors, such as monoclonal antibodies, are already commercially available.
In 2015, when describing his ADR grant, Dr. Campbell said, “We believe our project focuses on an area of Alzheimer’s disease pathology that has remained largely unexplored to date,” and that findings associated with the project could potentially lead to a novel Alzheimer’s therapies. Now, after much additional work, he and colleagues are closer to reaching that goal and are collaborating with a Japanese company to develop drugs that either inhibit or enhance claudin-5’s gatekeeping function.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
Every Donation is a Step Forward in the Fight Against Alzheimer’s
Your donation powers cutting-edge research and helps scientists explore new treatments. Help bring us closer to a cure and provide valuable information to the public.
Donate Today