Treatments for Glaucoma
Your doctor should help you decide which medications are best suited for you based on your case of glaucoma, medical history, and current medication regimen. Continue reading for different types of medications and treatments for glaucoma.

Support Vision-Saving Research
More than 4 million Americans are living with glaucoma. Your gift can help fund research that could protect their sight and provide valuable information to the public.
Common Treatments for Glaucoma
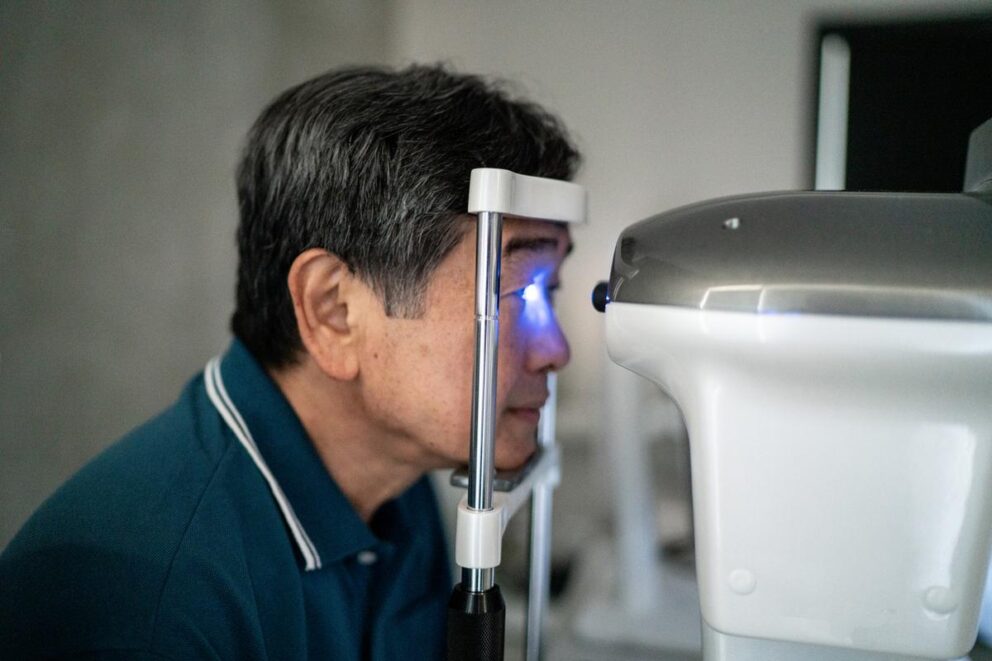
Eye drops are the most common treatment for glaucoma. The best treatment for you will depend on the type of glaucoma you have, its severity, and how well you respond to drugs, laser treatment, or surgery. While some types of glaucoma require different approaches, most therapeutic strategies attempt to lower intraocular eye pressure (IOP), the main risk factor associated with most types of glaucoma.
Top Questions to Ask Your Eye Doctor
Explore helpful tips to help you prepare for a conversation with your eye doctor.

Glaucoma Eye Drops
The eye, like the brain, protects itself with a barrier against potentially harmful substances. This blood-ocular barrier makes it difficult for pills or injections to travel through the bloodstream. As a result, most glaucoma medications are topical, meaning they are applied to the eye’s surface using eye drops or ointments, which are absorbed into the eye’s circulation.
Doctors use several types of eye drops to treat glaucoma, categorized below by their active ingredient. They either decrease the amount of fluid (aqueous humor) in the eye or improve its outward flow, and some do both. Sometimes doctors will prescribe a combination of eye drops. Your doctor should help you decide which medications are best suited for you.
Types of Glaucoma Surgeries
Surgery is an effective way to lower intraocular eye pressure, and, in some cases, can normalize pressure for some time without using medications. However, surgery is rarely chosen first as a treatment option due to the risk of complications. Another reason is the consequences of a poor outcome, while extremely rare, tend to be graver with surgery than with medications. For this reason, your doctor is likely to recommend surgery only if you are unable to use eyedrops or other medications, or if they don’t work well enough on their own to lower IOP. Most surgical procedures for glaucoma lower IOP by reshaping tissue to clear blockages, or by opening new channels for aqueous humor to drain. Less frequently, surgery is used to decrease aqueous humor production by refashioning the ciliary body, the part of the eye where aqueous humor is produced.
Laser Surgery
Laser surgery is the most frequently used procedure to treat open-angle, angle-closure, or neovascular glaucoma. It normally lowers eye pressure, but the length of time that pressure remains low depends on many factors, including:
- Age of the patient
- Type of glaucoma
- Other medical conditions that may be present
Many cases still need continued medication but possibly in lower amounts. The most common side effects of laser surgery are temporary eye irritation and pain, blurred vision, and a small risk of developing cataracts.
Your doctor may use laser surgery to treat open-angle, angle-closure, or neovascular glaucoma. He or she will perform laser surgery on an outpatient basis in the office or clinic after numbing your eye.
Traditional Surgery
In comparison, eye doctors often use conventional surgical procedures (also called incisional therapies) for glaucoma after other treatment strategies, such as medications and laser surgery, have failed.
When deciding on a treatment option, an ophthalmologist will take into account the unique aspects of each person’s case, including:
- The severity of the disease
- Response to medication
- Other health issues
Types of Laser Surgery
Trabeculoplasty
The most common laser procedure used for open-angle glaucoma, this procedure facilitates easier drainage.
Laser Peripheral Iridotomy
Laser peripheral iridotomy is frequently used to treat angle-closure glaucoma, in which the angle between the iris and the cornea is too small and blocks fluid flowing out of the eye. A laser creates a small hole in the iris to allow fluid drainage.
Cyclophotocoagulation
Cyclophotocoagulation is usually used to treat more aggressive or advanced open-angle glaucoma that has not responded to other therapies. Your doctor directs a laser through the sclera or endoscopically at the eye fluid-producing ciliary body. The procedure helps decrease the production of fluid and lower eye pressure. Patients often need multiple treatments.
Scatter Panretinal Photocoagulation
This laser procedure destroys abnormal blood vessels in the retina that are associated with neovascular glaucoma.
Types of Traditional Glaucoma Surgery
Preparing for Surgery and Recovery
Your doctor is responsible for evaluating and documenting your need for surgery, explaining its risks and benefits, and obtaining informed consent—which shows you understand and give your permission. They should review all your current medications and rule out allergies to any anesthesia and/or antibiotics that may be used.
Ask for detailed written instructions about where your surgery will occur and “dos and don’ts” in the days before and after the procedure. You won’t be able to drive home, so someone needs to accompany you or pick you up from the hospital or surgical center.
In the days following the procedure, your eye will be sore and bruised, and your vision may be blurry. That should clear up within a couple of weeks. Written discharge instructions should alert you to signs of infection, or other dangers. They should also give the time and place of your follow-up appointment.
Secondary Glaucoma Treatment
Secondary glaucoma is a broad term that encompasses many types of glaucoma that are the result of certain medical conditions in the eye or the body.
Frequently Asked Questions
Who Is At Risk of Developing Glaucoma?
Glaucoma is a leading cause of blindness among African Americans and Hispanics in the U.S. Three times as many African Americans have glaucoma than white populations. Glaucoma is 15 times more likely to cause blindness in African Americans between the ages of 45 and 64 than in white populations. All people older than 60 are at a greater risk of developing glaucoma than younger people.
Is There a Cure for Glaucoma?
Scientists are working toward a cure, but in the meantime, there are sight-saving treatments. That’s why the sooner glaucoma is detected and treated, the better the chance vision can be preserved.
Search for Glaucoma Clinical Trials
Clinical trials are crucial to advancing the most effective medical approaches. Today’s studies will lead to new standards of care in the future.

Resources
Recent Resources & Information

Expert Information
Can Stem Cell Treatments Cure Glaucoma?
In clinical trials, stem cell therapy for glaucoma shows promise for rebuilding the eye’s drainage system and protecting the optic nerve.

Glaucoma Chats
Implants and Injectables for Glaucoma Treatment
Discover the latest innovations in glaucoma treatment, from surgical implants to sustained-release medications.
Glaucoma Chats
Glaucoma Explained: Types, Risk Factors, and Treatments
Join us for an insightful conversation with Dr. Jaehong Han about the different types of glaucoma, including open-angle, angle-closure, normal-tension, and more, discussing who is most affected by each and how treatments can vary.

Podcast
Glaucoma Treatments in 2024
A glaucoma specialist discussed the diverse landscape of glaucoma treatments, including newly approved medications.

Glaucoma Chats
Latest Updates on Glaucoma Eye Drops
Dr. Natasha Nayak Kolomeyer, glaucoma specialist and ophthalmologist at Wills Eye Hospital, discusses various types of eye drops used in glaucoma treatment, how they work, potential side effects, and tips for managing challenges associated with their use.

Downloadable Resource
Treatments for Glaucoma
Read and download a printable fact sheet about the various types of glaucoma treatments.


