Clinical Trials and Research Studies
Clinical trials are clinical research studies using volunteers (also called participants) that aim to determine whether a medical strategy, treatment, or device is safe for use or consumption by humans. These studies may also present which experimental approach proves most effective for specific conditions or groups of people. Today’s clinical trials will lead to new standards of care. Learn more about clinical trials and how to get involved.
Search for a Clinical Trial
We connect researchers to people living with Alzheimer’s disease, macular degeneration, geographic atrophy, and/or glaucoma for interviews, focus groups, surveys, and more. Select a disease to get started.

How Do Clinical Trials Work?
Clinical trials play a critical role in the development of new treatments. They are the culmination of years—often decades—of work done by researchers to find ways to slow, treat, or even cure diseases. Unlike earlier research phases, clinical trials completely depend on volunteer human participants.
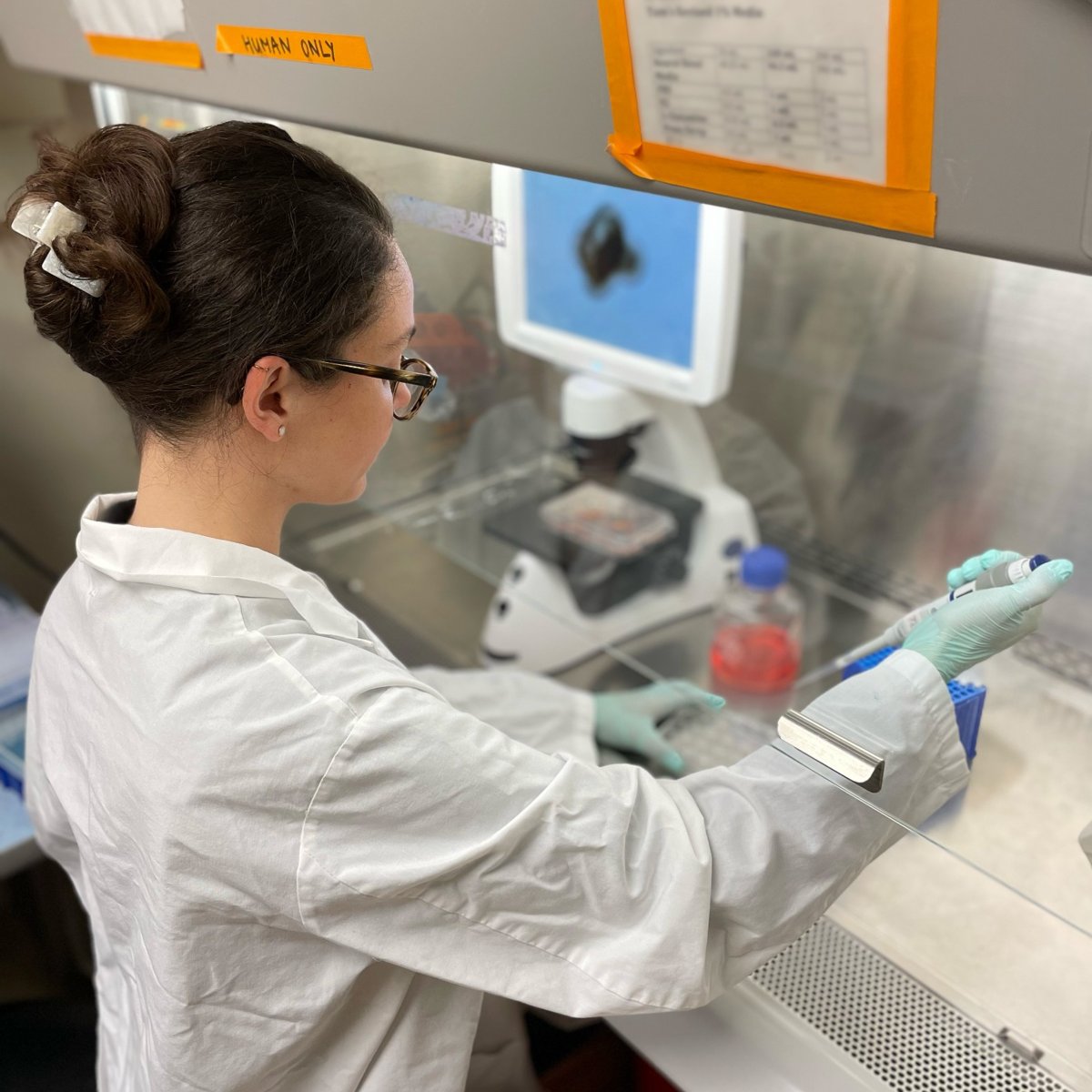
Starting in the Lab
Discovering a new treatment starts in the laboratory. It often takes several years to sift through thousands of potential treatments to find those fit to enter clinical trials.
Clinical Trial Phases
FDA Approval Process
The U.S. Food and Drug Administration (FDA) only approves drugs that it determines have solid evidence of safety and effectiveness for public use or consumption.
Enrolling in a Clinical Trial
Both people with a medical condition and healthy individuals may consider participating in clinical trials. Each trial has its own protocol (set of guidelines), and volunteers first must meet certain criteria to qualify for enrollment.
By enrolling in a clinical trial, a participant is making a noble effort to help test whether a candidate therapy (i.e. drugs, devices, or other study topics) has the potential to become a future drug, device, diagnostic test, prevention, or treatment for a particular disease or medical condition.
Volunteering for a clinical trial is also a way for participants to become actively involved in their own healthcare. But remember, there may be side effects, the treatments may not be effective, and participation will require a time commitment. It’s a decision that should involve a wider discussion with caregivers and doctors.
Before making a decision and giving informed consent, each person should seek as much information as possible about the trial and seriously consider the benefits and risks of volunteering. It is important to remember that a clinical trial is not a treatment, and the results of the trial could determine that the new treatment may not be better than the current standard of care.
Check out these additional resources below.
How to Leave a Clinical Trial
Participation in a clinical trial is voluntary, which means you can leave a clinical trial at any time.
Before leaving a clinical trial, notify the research team and provide the reasons for leaving the study. This will help the team to prepare information for their detailed report on the clinical trial to the FDA.
Depending on the type of study, leaving can be simple, with just a few requirements to complete before returning to regular care. However, close monitoring may be required in some other cases until the participant is safely off the study drug or until regular care can be resumed.
Ongoing Clinical Trials and Research Studies
Learn more about ongoing clinical trials.
- Alzheimer’s
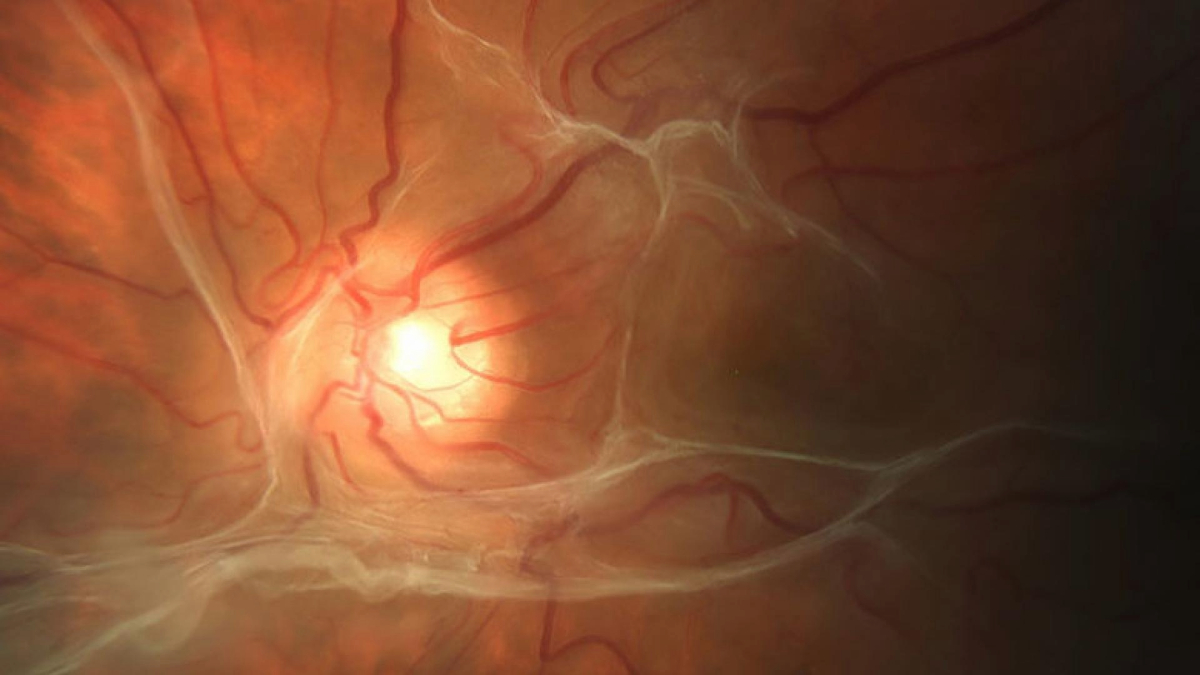
- Macular Degeneration
- Macular Degeneration Research, a BrightFocus Foundation program, has partnered with Kyowa Kirin, a pharmaceutical company actively searching for volunteers with neovascular (or “wet”) age-related macular degeneration to participate in a Phase 2 clinical trial for a novel investigational eye drop, KHK4951. Click here to find more information.
- Geographic Atrophy
- Glaucoma
Related Resources

Expert Information
Talking with Your Doctor About Clinical Trials
Read helpful questions to ask the research team and/or healthcare professional associated with a clinical trial.

Downloadable Resource
Clinical Trials: Your Questions Answered
This brochure covers what clinical trials are, what volunteering for a trial means to you, what you should consider before participating, and how you are helping researchers impact the lives of millions of people.