
African Americans and Hispanics are at increased risk of developing glaucoma. Find out why and learn about important steps you can take to prevent vision loss.
Glaucoma is a leading cause of irreversible blindness. Unlike cataracts, the leading cause of blindness worldwide which can be “cured” with cataract surgery, there is no way to reverse vision loss due to glaucoma. Further, researchers estimate that half of all people with glaucoma do not know that they have it. This is because the most common form, open-angle glaucoma, has no symptoms, earning it the nickname the “silent thief of sight.”
Primary open-angle glaucoma affects an estimated 2 to 3% of U.S. adults age 40 and older, and the prevalence is predicted to increase as the population skews older over time. More than 3 million U.S. adults over 40 have glaucoma; of these, an estimated 2.72 million have open-angle glaucoma, the most common form of this disease. By 2030, more than 4 million U.S. adults over 40 are predicted to have glaucoma; this number is expected to increase to over 6 million by 2050.
The Leading Cause of Blindness in African Americans
Open-angle glaucoma is the leading cause of irreversible blindness in African Americans.
Based on data analyzed in 2012, more than 520,000 Americans with open-angle glaucoma are African American.
One of the landmark studies to examine the prevalence of open-angle glaucoma in the African American community was the Baltimore Eye Survey, whose results were published in 1991.
This study showed that the prevalence of glaucoma was 4% in African Americans ages 50-59 and increased to approximately 13% in African Americans ages 80-89. Adjusting for age, African Americans were 3 to 4 times more likely to have a diagnosis of glaucoma compared to Caucasians. Not only was the overall prevalence higher in African Americans, but the disease began at an earlier age. This study also showed that half of all patients, regardless of ethnicity, were unaware that they had glaucoma.
Why Are African Americans at Increased Risk?
Why are African Americans more likely to be diagnosed with glaucoma at a more advanced stage of disease and lose vision caused by open-angle glaucoma compared to non-Hispanic whites? The reasons are unclear, but social determinants of health and health disparities may contribute.
Social determinants of health are the conditions where people are born, live, work, and age that impact their health risks and outcomes. Research has shown that different socioeconomic groups and/or racial/ethnic groups do not receive the same level of medical care. For example, in a study of patients with Medicaid or commercial insurance, the researchers found that Medicaid patients were much less likely to receive common glaucoma tests compared to patients with commercial insurance.
Furthermore, disparities in testing were observed across all racial/ethnic groups but was worse for African American patients. This is particularly concerning since African Americans are more likely to go blind from glaucoma than white patients.
Overall, in the African American population, open-angle glaucoma is more common, more difficult to treat, and more severe at the time of diagnosis, which results in more blindness.
Glaucoma Risk in the Hispanic/Latino Community
Hispanic/Latinos are another ethnic group that shows an increased risk of open-angle glaucoma. The Los Angeles Latino Eye Study (LALES) studied the prevalence of eye diseases in Latinos, with most of the patients in this study being of Mexican ancestry. The prevalence of open-angle glaucoma in Latinos (approximately 5%) was found to be similar to that of African Americans.
The study found that 75% of Latinos with glaucoma were previously undiagnosed, which may be attributed to the large percentage of patients who did not have health insurance. The study also supported earlier findings that suggest that monitoring blood pressure is extremely important in patients with glaucoma. Patients with very high blood pressure have higher eye pressure, which is known to be a major risk factor in open-angle glaucoma. On the other hand, patients with very low blood pressure also have increased risk of open-angle glaucoma, which is thought to be related to poor blood flow to the optic nerve.
Another recent study estimated that the majority of the more than 2.7 million people with open-angle glaucoma in the U.S. are people aged 70 to 79 years, women, and non-Hispanic whites. However, by 2050, researchers estimate that more than 7.3 million people will have open-angle glaucoma, with the highest number still among people ages 70 to 79 years and women, but there will be a shift to Hispanics. Notably, this study predicted that the largest demographic group with glaucoma will be Hispanic men.
Decreasing Your Risk
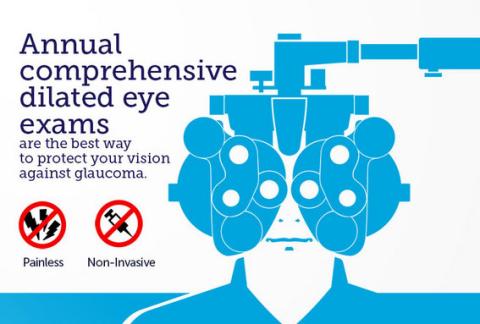
So what should you do? The best defense against blindness related to glaucoma is having a comprehensive, dilated eye exam. Since glaucoma is age-related, and the diagnosis is often made over a period of time as the eye doctor monitors you, it is worth having a baseline examination by age 40.
It is also important to consider whether you have other risk factors for open-angle glaucoma, including being over 40, high eye pressures, a family history of glaucoma, very high or very low blood pressures, extreme nearsightedness, or diabetes. If you have one or more of these risk factors, a comprehensive eye exam including pupil dilation is advisable. The National Eye Institute also recommends that people of African ancestry age 40 and older should be evaluated for glaucoma, or even earlier if there is a family history of glaucoma. They also recommend that people of Hispanic ancestry be evaluated for glaucoma by age 60.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Health Equity
- Risk Factors









